Key points
- IDDSI is a language, not a law, it enables clear descriptions of textures based on evidence and rigorous testing rather than subjective descriptions
- Clinical judgement remains key, the IDDSI level(s) recommended should meet the individual’s needs based on clinical assessment and discussion with key individuals
- IDDSI is person-centred – defining an IDDSI level is helpful to describe the maximum level they can safely tolerate.
- IDDSI does not restrict the person to a level alone, previous levels may also be deemed appropriate to open up choice and different textures
- IDDSI is used as one system for describing food and fluid modification, regardless of the reason why the individual needs their food or fluid modified
- It is aimed to be used across all age ranges and cultures
Introduction
Here you will find information about the International Dysphagia Diet Standardisation Initiative (IDDSI) Framework.
Frequently asked questions
- FAQs developed by IDDSI
FAQs on implementing the IDDSI Framework (March 2018)Related clinical topic areas:
Dysphagia
Related delivering quality services topic areas:
- Care pathways
- Collaborative working
- Consent
- Delegation
- Duty of care
- Enabling service users, families and carers
- Having difficult conversations
- Local influencing
- Managing risk
- Outcome measurement
- Professional accountability and autonomy
- Raising awareness
- Service planning and improvement
- Supported decision making and mental capacity
- Upskilling the wider workforce
The IDDSI Framework
The International Dysphagia Diet Standardisation Initiative (IDDSI) Framework is an international set of descriptors describing texture modified foods and thickened liquids for people with eating, drinking and swallowing problems (dysphagia) across the lifespan.
It was developed by an international group of volunteers from a variety of professions, including nutrition and dietetics, medicine, speech and language therapy, occupational therapy, nursing, patient safety, engineering and food science and technology. These individuals form the IDDSI Board.
The framework consists of a continuum of 8 levels (0-7):
- Drinks: Level 0-4
- 0 – Thin
- 1 – Slightly thick
- 2 – Mildly thick
- 3 – Moderately thick
- 4 – Extremely thick
- Foods: Levels 3-7
- 3 – Liquidised
- 4 – Pureed
- 5 – Minced and moist (transitional foods)
- 6 – Soft and bite-sized (transitional foods)
- 7 – Regular/easy to chew (transitional foods)
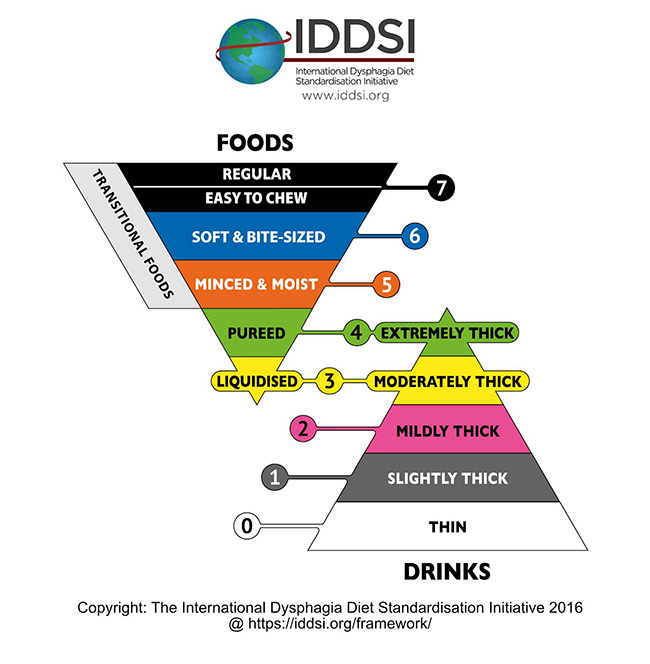
For more information about the different levels, please visit IDDSI’s website.
Level 7 Easy to Chew
IDDSI conducted a survey in June-July 2018 to address a number of queries they had received regarding the need for a label and testing methods for foods that are ‘soft’ but not necessarily served in ‘bite-sized’ pieces (e.g. without particle restrictions).
Following the results of the survey, the IDDSI Board agreed to develop a new subcategory, Level 7 Easy to Chew.
Below are some frequently asked questions that RCSLT members ask about this subcategory that IDDSI have answered.
What is Level 7 Easy to Chew?
It is a subcategory of Level 7 Regular and describes softer food choices that fall within Level 7 Regular.
How is Level 7 Easy to Chew foods determined?
There is a specific test for ‘soft’ which involves using a table fork to compress the material, applying a light pressure just sufficient to cause the thumbnail to blanche. The food should crush easily and deform through the fork prongs, and not return to its original shape when pressure is removed.
Is this subcategory suitable for individuals with dysphagia?
As with all texture modification strategies, clinical judgement is required to decide which categories of foods are suitable for which individuals. IDDSI advise that Level 7 Easy to Chew is intended for those who do not require particle size restriction to help reduce choking risk, in order to highlight the key difference between Level 6 and L7EC. If an individual has an increased risk of choking on foods, this level would not reduce that risk in itself, however it may form part of a risk-managed approach to eating & drinking in the presence of dysphagia.
A person who is able to eat foods within this subcategory can have dysphagia. In particular, it is possible that someone may have dysphagia affecting their ability to drink thin liquids, but would not have a need for particle size restriction involved in Level 6.
This category of foods is widely used by individuals who do not have swallowing problems which would be labelled dysphagia. For example, this subcategory is useful for individuals who may have transient difficulties with chewing resulting from having had oral or jaw surgery. In this instant, Level 7 Regular would not be appropriate.
Why is it a subcategory of Level 7 and not Level 6? A carer might interpret Level 7 Easy to Chew as a Level 7 Regular and the person given it may be at an increased risk of choking due to no particle restriction.
IDDSI chose to have this softer option as part of Level 7 as they wanted to avoid the risk of someone on Level 6 (possibly with an identified risk of choking) being given a ‘Level 6 Easy to Chew’ accidentally. This risk would be more severe to the person who is consuming the food.
Level 6 is very safe as its particle size restriction means that food particles would not be large enough to block the airway completely, but it is restrictive. In comparison, Level 7 Easy to Chew does not have this risk mitigation built in, making it a subcategory of Level 7 and not Level 6.
Resources
‘A bit of background on Regular 7 Easy to Chew’, IDDSI e-bite, May 2019
RCSLT involvement
The decision to adopt the IDDSI Framework
The group spent over a year gathering evidence to determine whether or not to adopt the IDDSI Framework. This work included literature reviews, pilots, a pros and cons exercise and surveys of healthcare professionals. The RCSLT and the BDA consulted with expert advisors and their members through surveys disseminated via member networks. The results of these surveys informed the decision by both organisations to adopt IDDSI in October 2017. The RCSLT and the BDA provided updates via their professional magazines to members on this work.
The UK Expert Reference Group agreed to a phased implementation plan which commenced in April 2018 with full implementation by April 2019.
The UK Expert Reference Group has now ceased to exist.
Continued RCSLT involvement
Why use the IDDSI Framework?
There are many benefits of using the IDDSI Framework. Some of them are:
- Each level is based on evidence. The previous UK descriptors were based on a consensus of expert opinion, not research evidence. For more information on how the Framework was developed, see IDDSI’s website and the peer-reviewed publication in the journal ‘Dysphagia‘.
- The testing methods of the levels are scientific and designed so that they are easy to use. For more information about IDDSI testing methods, see the IDDSI Flow Test for testing drinks and the different food testing methods on IDDSI’s website.
- Patient safety: NHS Improvement has recommended using IDDSI terminology to reduce choking incidents in their patient safety alert. As there are levels to describe both foods and liquids, this means that the safety of patients when both eating and drinking is accounted for.
- The framework is prescriptive, not restrictive. Patients should be prescribed all levels they can manage safely, which gives them a great variety of foods they can eat and drink and as such improves their quality of life.
- The framework is being implemented worldwide. This means that when healthcare workers and patients travel from country to country there will be no confusion about the dysphagia descriptors being used and patients remain safe.
- The data on dysphagia improves. As more countries use the same descriptors, the ability to do larger research studies and systematic reviews is much greater. This means that more robust evidence about the care of patients with dysphagia can be generated.
Resources
- NHS Improvement Patient Safety Alert (jointly developed with RCSLT and BDA): Resources to support safer modification of food and drink (27 June 2018)
- Why adopt IDDSI? (PowerPoint)
- Comparing the UK National Descriptors with IDDSI (both liquids and foods) (PowerPoint)
- UK National Descriptors: Different interpretations (YouTube)
Tips on Implementation
Implementation of the IDDSI Framework will look different depending on the size of the organisation, number of suppliers involved, management support and staff engagement. Communication about IDDSI needs to be far-reaching and accessible to all health and social care professionals and staff, including community pharmacists, GPs and care home workers.
The RCSLT recommends the below actions at a local level to support a system-wide approach to implementation and to maximise patient safety. They have been extracted and edited as appropriate from a joint statement developed with the British Dietetic Association in April 2018. Access the full statement under Resources below.
- Raise concerns about patient safety risks through your organisation’s governance structures, e.g. Quality Patient Safety Governance. This way the concerns will be appropriately assessed with a risk score before and after mitigation.
- Escalate the need for a co-ordinated system-wide approach to developing a local implementation plan at board level within your organisation. This may be through Directors of Nursing, AHP Leads, Head of Quality or equivalent. This plan would need to include a range of stakeholders, including local care homes, Clinical Commissioning Groups (CCGs), other NHS organisations, GP practices and community pharmacies.
- Contact the relevant manufacturers to raise any concerns directly, and work together with them to ensure that patients/service users continue to receive great care and are not at risk of harm. The person contacting them could be yourself or the appropriate senior manager. Given the range of thickener products available, some service providers are considering whether to change products to one that they consider is more suitable.
- Check with your employer to see whether they have been offered support by contracted manufacturers to use their products, including training and a helpline.
- Include manufacturers in your whole system approach to implementation. This has been found effective by manufacturers who have been involved with early adopters, who are also committed to supporting the development of local implementation plans. This includes training for staff to help with the transition to any changes in instructions on the use of products in line with IDDSI.
- Check out the case studies from Greater Glasgow and Clyde, Hull and East Yorkshire and East Sussex under Learning resources. They have used a whole system approach to implementation.
- Include pharmacy and medicines management departments to support implementation particularly in community to ensure a process for transition for patients no longer under the care of speech and language therapy who are using a thickening agent on prescription.
- Do not underestimate the amount of training and information sharing required to inform staff and key stakeholders about IDDSI. Utilise all available platforms for sharing information on a regular basis.
- Support approaches to implementation of IDDSI by:
a. Join IDDSI to access the latest information, including resources and training, e.g. webinars
b. Check these webpages for updates regularly.
c. Set up and attend relevant RCSLT Clinical Excellence Network (CEN) meetings to support the sharing of best practice. See a full list of CENs here.
d. Contact us to share best practice approaches and resources.
e. Work together with other colleagues in your region to support implementation.
f. Contact us if you have any concerns about the IDDSI Framework.
Resources
Tips on using the IDDSI Framework
The RCSLT recommends the following tips on using the IDDSI Framework.
- Use your clinical judgement first and foremost when making recommendations for texture modification or fluid modification for the service user
- Use IDDSI as the starting point to describe what modified texture and fluids the service user can safely consume
- Consider the whole range of IDDSI Levels that the service user can safely manage in your recommendation. It is important to give them the least restrictive option to allow a diet that is as interesting and varied as possible, taking into account health, wellbeing and quality of life.
- Personalise your recommendation so that it fits with the needs and wishes of the service user, but refer to IDDSI in your case notes, reports, clinical documentation and in any professional correspondence. It is important that the description and recommendation for the food and fluid modification is right for that service user and not driven by IDDSI.
- Allow the service user and their carer(s)/family to use terminology that is suitable to them – it must be meaningful to them. However, as stated above, refer to IDDSI in any written material that is communicated to the wider healthcare team so that other professionals understand the recommendations that have been made.
Learning resources
Here you will find a range of learning resources which supports implementation of the IDDSI Framework in addition to those mentioned in the other sections. If you have resources that you are able to share, please Contact us.
IDDSI-developed resources
IDDSI has developed a number of resources that you may find useful. Please visit their IDDSI Resources section to find out more.
Case studies
RCSLT and BDA Statement Annex A: NHS Greater Glasgow and Clyde and East Sussex
Webinar
RCSLT and IDDSI webinar: Making IDDSI work for you (13 February 2019)
Journal articles
Cichero, J.A.Y., Lam, P., Steele, C.M. et al. (2017). Development of International Terminology and Definitions for Texture-Modified Foods and Thickened Fluids Used in Dysphagia Management: The IDDSI Framework. Dysphagia,32 (2), 293-314. https://doi.org/10.1007/s00455-016-9758-y
Steele, C.M., Alsanei, W.A., Ayanikalath, S. et al. (2015). The Influence of Food Texture and Liquid Consistency Modification on Swallowing Physiology and Function: A Systematic Review. Dysphagia, 30 (1), 2-26. https://doi.org/10.1007/s00455-014-9578-x
PowerPoint presentations
YouTube videos
Explanation of the UK perspective of the IDDSI Framework
RCSLT member-developed resources
Harrogate and District Foundation Trust – ALD Speech and language therapy
Patient-friendly leaflets
- IDDSI Level 3 (PDF)
- IDDSI Level 4 (PDF)
- IDDSI Level 5 (PDF)
- IDDSI Level 6 (PDF)
Lewisham and Greenwich NHS Trust
Patient-friendly leaflets
- IDDSI Level 1 & IDDSI Level 5 (Word)
- IDDSI Level 2 & IDDSI Level 4 (Word)
- IDDSI Level 2 & IDDSI Level 6 (Word)
Dietetic supplements
Posters and charts
- Kitchen poster (Microsoft Publisher)
- Diet conversion chart (Microsoft Publisher)
- Thickener conversion chart (Microsoft Publisher)
Hull and East Yorkshire Hospitals NHS Trust
Posters and charts
Flyer
Letters
Whittington Health NHS Trust – LD speech and language therapy
Level descriptions
- IDDSI descriptions at a glance (Word)
- Level 1 (Word)
- Level 2 (Word)
- Level 3 (Word)
- Level 4 (Word)
- Level 5 (Word)
- Level 6 (Word)
Level instructions
East Sussex Healthcare NHS Trust
Patient-friendly flyers
- Product instructions – known Stage 1 (old UK National Descriptors) (PDF)
- Product instructions – known Stage 2 (old UK National Descriptors) (PDF)
- Product instructions – known Stage 3 (old UK National Descriptors) (PDF)
- Product instructions – unknown stage (old UK National Descriptors) (PDF)
Level descriptions and instructions
- Level 3 (Word)
- Level 4 (Word)
- Level 5 (Word)
- Level 5 – how to prepare a sandwich (Word)
- Level 6 (Word)
Conversion chart
Leaflet
- IDDSI leaflet (Microsoft Publisher)
Information sheet for practitioners
- High risk foods to avoid (Word)
Templates
Keep up-to-date with the latest developments of IDDSI
News items
- IDDSI: Update on 10ml syringes used for flow test (10 April 2019)
IDDSI ebites
IDDSI has a monthly enewsletter providing the latest information about the Framework. To receive the latest news please subscribe here.
Contact IDDSI directly
If you have any questions directly related to the Framework, please contact office@iddsi.org.
Please contact us if you have any other questions.



