Key points
- Risk management is recognising which events (hazards) may lead to harm, minimising their likelihood (how often) and consequence (how bad)
- Both individual practitioners and organisations have a responsibility to manage risk.
- Speech therapists need to be able to identify and appropriately manage potential risks to themselves and others, across all areas of their work
- Specific risk management requirements may vary across settings.
- Practitioners should seek help and/or advice if the situation is something beyond their experience or competence.
- Effective use of clinical supervision, and knowing when to seek help in managing a risky situation so it doesn’t escalate, are essential to effective risk management
Introduction
The RCSLT encourages members to consider “risk” across all areas of their work and practice, in accordance with relevant HCPC standards of conduct, performance and ethics.
At times individual practitioners will need to adhere to more than one policy, e.g. NHS provider working in schools. At other times individual practitioners will need to develop their own policies and procedures for the management of risk within their practise.
Here you will find guidance to support you to manage risks, associated with your clinical and professional practice appropriately.
These pages cover guidance on:
- Responsibilities
- Organisational responsibilities
- Description of risk types
- Clinical risk assessment
- National guidance
- Resources
Please note
These web pages do not identify / address every individual risk that may be associated with speech and language therapy practice. For risks relating to specific client groups and settings, please visit the Clinical A-Z .
Further information on managing risk
Related topics
- Continuing professional development
- Dealing with the media
- Delegation
- Duty of care
- Evidence-based practice
- Evolving roles & advanced clinical practice
- Information governance
- Supported decision making and mental capacity
- Professional accountability and autonomy
- Safeguarding
- Supervision
- Technology for SLTs
- Clinical A-Z
Please contact us with any feedback on these pages.
Responsibilities
All practising SLTs have a professional responsibility to manage risk as stated in the HCPC Professional Standards
HCPC standards of conduct, performance and ethics
Identify and minimise risk
6.1 You must take all reasonable steps to reduce the risk of harm to service users, carers and colleagues as far as possible.
6.2 You must not do anything, or allow someone else to do anything, which could put the health or safety of a service-user, carer or colleague at unacceptable risk.
Manage your health
6.3 You must make changes to how you practise, or stop practising, if your physical or mental health may affect your performance or judgement, or put others at risk for any reason.
See also:
- Key Area 7 – Report concerns about safety
- Key Area 8 – Be open when things go wrong
- Key Area 9 – Be honest and trustworthy
As in all areas of practise, individual practitioners should seek help and/or advice if the situation is something beyond their experience or competence.
Effective use of clinical supervision, and knowing when to seek help in managing a risky situation so that it doesn’t escalate, are essential elements of effective risk management.
Terminology
The following covers key terms in relation to managing risk, which are used throughout this guidance.
A clinical risk or healthcare risk
The chance of an adverse outcome resulting from clinical investigation, treatment or patient care
Clinical risk management
This can be defined as “The actions taken, on the basis of a risk assessment, that are designed to prevent or limit undesirable outcomes.” (Department of Health, 2007a, citing Mersey Care NHS Trust, 2006).
Hazard
Situations with the potential to cause harm
Can be described as balancing the risks and benefits of one course of action against another. A positive risk-taking approach acknowledges that risk taking can have benefits for some individuals, balancing necessary levels of protection with preserving reasonable levels of choice and control (Think Local Act Personal, DOH, 2011)
Decisions about risk management are made with the aim of improving the service-user’s quality of life and plans for recovery; however, the organisation should remain aware of the safety needs of the service-user, their carer and the public.
Positive risk management means being aware that risk can never be completely eliminated, and being aware that management plans inevitably have to include decisions that carry some risk. This should be explicit in the decision making process and should be discussed openly with the service-user and/or their carer. (Document for clinical risk assessment & management).
Risk
The probability that a specific adverse event will occur in a specific time period, or as a result of a specific situation
Risk Assessment
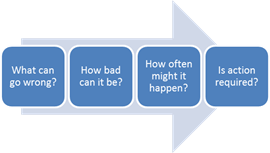
Identifying what can go wrong, how bad it can be, how often it might happen, who it might happen to, and whether action is required.
Risk management
Risk Management in healthcare includes the whole spectrum of things that could and can go wrong. It includes slips, trips and falls involving staff, patients/clients and the public, administrative errors that impact on patient/client care and clinical incidents that have a direct effect on the outcome of patient/client care. It will also include the management of the business risks associated with running a NHS Board or hospital including financial, ethical and information technology risks. (Flying Start, 2018)
Organisational Risk Management
This information will be particularly relevant to practitioners working in independent practise or working in a role where they have responsibility for managing risk at an organisational level.
Risk management at an organisational level is the process by which an organisation evaluates and reduces its risk exposure. Because the environment is dynamic, risk cannot be completely eliminated within any organisation, however it can be managed.
Each organisation must decide its own risk-tolerance, taking into consideration relevant:
- current legislation
- current clinical guidance
- clinical governance requirements
The Health & Safety Executive has developed guidance to support organisations to manage risk; these are called Managing Risks.
Business planning and risk management should not be separate activities. Action plans to manage risks and enhance opportunities should be developed and incorporated into business plan reports and kept regularly up-to-date.
Once an Organisational Risk Management Plan is in place, it is necessary to ensure that it remains effective.
There are four elements to maintaining the effectiveness of risk management practices:
- Identify who will be responsible for risk management within the organisation
- Keep procedures up to date:
Over time, circumstances change and your risk management plan may become inappropriate. Experience gained from implementing risk management procedures can be used to further refine those procedures. Also, better procedures might emerge which can be used to replace less effective procedures.
3. Re-assess risks:
The risks you identified in your risk management plan, and your assessment of them, were probably fairly accurate at the time you did the plan. Twelve months later it is more than likely that some of those risks will have changed.
There are two ways that you can ensure that your risk management plan is up to date:
a) Review on a regular basis. The more changeable your organisation and/or its environment, and the higher the level of risk you face, the greater the need to keep your risk management plan up to date. At a minimum, your risk management plan should be reviewed at least once a year.
b) Evaluate changes within your organisation, or within your organisation’s environment, in terms of their implications for risk within your organisation. New legislation relevant to your organisation, taking on new roles, acquisition of new equipment, or creation of new positions should all be considered for their implications for risk management.
4. Report on risk management, and this process should include:
- Description of any new risks
- The effectiveness of existing risk management practice (current mitigations)
- The occurrence of risks (accidents, theft, and so forth) during the reporting period
- Reporting on risk will normally be done by the person who has the responsibility for risk management. Risk reports should be filed and used in regular reviews of risks and procedures.
Developing policies & procedures to manage risk
Organisations will have different policies and procedures relating to the management of risk.
Healthcare policies and procedures are influenced by many factors. These factors include healthcare and legal regulations, evidence-based practices, and accreditation standards.
Policies and procedures should be written in a way that’s easy for front line staff to interpret and apply. Front line staff involvement in the writing of policies and procedures is also recognised as a critical component of effective policy and procedure development.
Policies and procedures should be written using a standardised writing format or style, so that staff members looking up any policy will know what section they need to go to for the right information. The organisation needs to choose a format and stick with it.
One published format for the writing of policies and procedures (Best Practises in Policies and Procedures, Stephen Page, 2010) consists of eight parts:
- Purpose
- Persons Affected
- Policy
- Definitions
- Responsibilities
- Procedures
- Document Approvals
- Change History
Identifying potential risks
“Risk management in healthcare includes the whole spectrum of things that could and can go wrong. It includes slips, trips and falls involving staff, patients/clients and the public, administrative errors that impact on patient/client care and clinical incidents that have a direct effect on the outcome of patient/client care. It will also include the management of the business risks associated with running a NHS Board or hospital including financial, ethical and information technology risks”. (Flying Start, 2018)
There are many different types of hazards that practitioners should consider when identifying areas of their practise and/or environment that may require specific risks assessments.
These can be categorised under three headings; risk to service-user (others), risk to practitioner and organisational risk, and examples of these hazards are described below:
Risk to service-users/others
- Clinical risks
- The chance of an adverse outcome resulting from clinical investigation, treatment or patient care
- Safeguarding concerns
- Some groups, such as children, the elderly and frail, and individuals with learning disabilities, are at particular risk of abuse and harm. Types of abuse include physical abuse, emotional abuse, sexual abuse, financial abuse, neglect, and domestic abuse.
- Information governance
- Food Hygiene
- Food hygiene/food safety standards are overseen by the Food Standards Agency
Risk to practitioner
- Risks to maintaining HCPC registration
- If a registrant does not meet HCPC standards, the HCPC can take action which might include stopping them from practising.
- Lone working risks
- Any situation or location in which someone works without a colleague nearby or when someone is working out of sight or earshot of another colleague. Examples of lone workers include: (not an exhaustive list)
-
- Staff in fixed establishments where:
- Only one member of staff works on the premises
- Staff working separately from others
- Staff working outside normal hours
- Staff working in other external locations
- Mobile lone workers working away from their base (when work may be carried out in):
- Client’s homes
- Nursing homes
- Other Organisations premises or Business premise
- Staff in fixed establishments where:
- Risks from violence and/or aggression
- The Health and Safety Executive (HSE) defines work-related violence as any incident in which a person is abused, threatened or assaulted in circumstances relating to their work. This can include verbal abuse or threats as well as physical attacks.
- Stress
- Work related stress develops because a person is unable to cope with the demands being placed on them. Stress, including work-related stress, can be a significant cause of illness and is known to be linked with high levels of sickness absence, staff turnover and other issues such as more errors.
- Risks associated with moving and handling
- This is a key part of the working day for most employees; from moving equipment, supplies or waste to assisting clients in moving/using restraint. Poor moving and handling practice can lead to back pain and musculoskeletal disorders (which can lead to inability to work) and moving and handling accidents (which can injure either the practitioner or the client)
- Sharps injuries
- These are a well-known risk in the health and social care sector. Sharps contaminated with an infected patient’s blood can transmit more than 20 diseases, including hepatitis B, C and human immunodeficiency virus (HIV). Because of this transmission risk, sharps injuries can cause worry and stress to the many thousands who receive them. (HSE)
Health & Safety Risks / Environmental Risks
- Slips, trips & falls
- These account for around half of all reported major injuries to employees. Some users of health or care services can be particularly vulnerable to falls injuries, and falls on the same level account for a significant number of injuries to service users – many of which are preventable.
- Infections at work
- COSHH (Control of Substances Hazardous to Health Regulations)
- This covers substances that are hazardous to health. Substances can take many forms and include:
- chemicals
- products containing chemicals
- fumes
- dusts
- vapours
- mists
- Nanotechnology
- gases and asphyxiating gases and biological agents (germs). If the packaging has any of the hazard symbols then it is classed as a hazardous substance.
- germs that cause diseases such as leptospirosis or legionnaires disease and germs used in laboratories
- This covers substances that are hazardous to health. Substances can take many forms and include:
- Fire safety
- At most workplaces the local Fire and Rescue Authority are responsible for enforcing general fire safety and if you need advice you should contact them.
- Legionnaires’ disease
- This is a collective term for diseases caused by legionella bacteria including the most serious Legionnaires’ disease. Legionnaires’ disease is a potentially fatal form of pneumonia and everyone is susceptible to infection. The risk increases with age but some people are at higher risk including:
- people over 45 years of age
- smokers and heavy drinkers
- people suffering from chronic respiratory or kidney disease
- diabetes, lung and heart disease
- anyone with an impaired immune system
- The bacterium Legionella pneumophila and related bacteria are common in natural water sources such as rivers, lakes and reservoirs, but usually in low numbers. They may also be found in purpose-built water systems such as cooling towers, evaporative condensers, hot and cold water systems and spa pools.
- If conditions are favourable, the bacteria may grow increasing the risks of Legionnaires’ disease and it is therefore important to control the risks by introducing appropriate measures.
- This is a collective term for diseases caused by legionella bacteria including the most serious Legionnaires’ disease. Legionnaires’ disease is a potentially fatal form of pneumonia and everyone is susceptible to infection. The risk increases with age but some people are at higher risk including:
Organisational Risks
- Strategic Risks
- External risks, which may affect your organisation such as changes in the environment in which you operate
- Financial Risks
- This covers financial risks facing the organisation in terms of internal systems, planning, funding etc
- Operational Risks
- This looks at the risks, which arise from the services you deliver or the activities you carry out
- Reputational Risk
- Risks to the reputation of the organisation
- Risks associated with people
- Risks associated with clients, the employment of staff, and the involvement of volunteers
- Regulatory Risks
- Risks associated with the legislative framework within which your organisation operates
- Governance Risks
- Risks that are part of the management of the organisation
To prevent harm it is important to understand not only what could go wrong, but also how and why it may go wrong.
Effective Risk Assessment
Being able to recognise potential hazards and identify potential risks is an essential element of effective risk management. To prevent harm it is important to understand not only what is likely to go wrong but also how and why it may go wrong.
Consider the activity within the context of the physical and emotional environment, and the culture of the organisation and the staff who perform the activity.
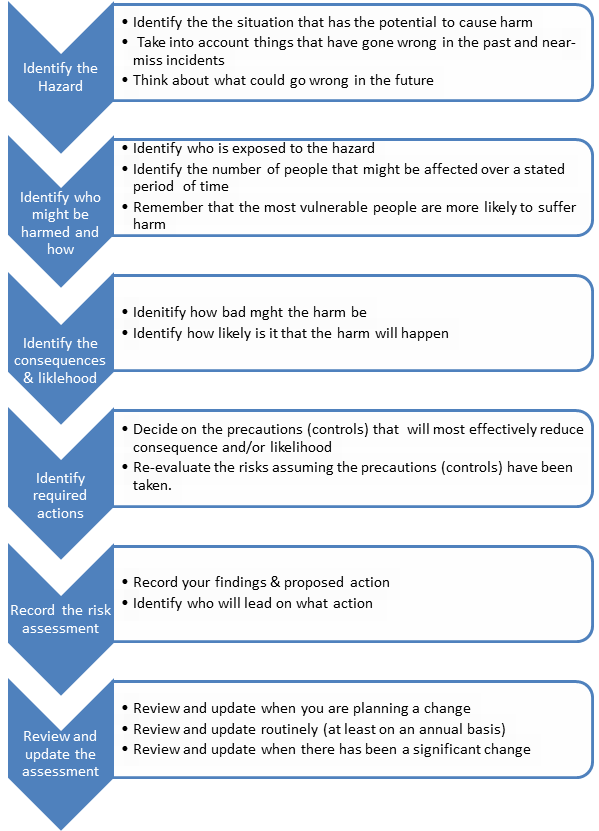
Effective risk assessment answers these key questions:
There are 6 steps to effective risk assessment:
- Identify hazard
- Identify who might be harmed and how
- Identify the consequences if this happened and the likelihood of it occurring
- Identify required actions
- Record the risk assessment
- Review and update the risk assessment
Risks are scored according to the likelihood of them occurring and the severity of the potential consequences
Additional Resources to Support Effective Risk Assessment can be found on the Risk Management – learning page
Steps for Effective Risk Assessment
The RCSLT suggest that all practitioners:
- Have a set of policies and procedures in place relating to the assessment and management of risk within their own organisation
- Take all reasonable steps to ensure health, safety and welfare of any person involved in any activity for which they are responsible.
Many organisations will have their own risk assessment forms but Healthcare risk assessment made easy (The Patient Safety Agency) explains the risk assessment process and has developed model forms which can be found on their website
The Health & Safety Executive also produced guidance regarding risk assessment, while they also provide risk assessment templates.
Depending on the risk being assessed, SLT’s may also have a role in supporting service user involvement in risk assessment, as well as integrating speech, language and communication needs of the patient in risk assessment and formulation for example, using an easier to read 5 p’s self-formulation with the patient
Example risk matrix
The National Patient Safety Agency (2008, NPSA) advised that the rating of risks is used to identify the level at which the risk will be managed in an organisation, assign priorities for remedial action, and determine whether risks are to be accepted.
In order to effectively rate an individual risk, the consequence(s) of that risk occurring and the likelihood of it occurring must both be considered.
Consequence
When undertaking a risk assessment, the consequence or ‘how bad’ the risk being assessed is must be measured. In this context, consequence is defined as: the outcome or the potential outcome of an event.
Clearly, there may be more than one consequence of a single event and these may range in severity.
Organisations have different definitions of the consequences and many issues need to be factored into the assessment of consequence, for example:
- Does the organisation have a clear definition of what constitutes a minor injury?
- What measures are being used to determine psychological impact on individuals?
- What is defined as an adverse event and how many individuals may be affected?
A single risk area may have multiple potential consequences, and these may require separate assessment. It is also important to consider from whose perspective the risk is being assessed (organisation, member of staff, patient) because this may affect the assessment of the risk itself; its consequences, and the subsequent action taken.
Likelihood
The likelihood score is a reflection of how likely it is that the adverse consequence described will occur. Likelihood can be scored by considering:
Frequency (how many times will the adverse consequence being assessed actually be realised?)
OR
Probability (what is the chance the adverse consequence will occur in a given reference period?)
Individual organisations / practitioners will need to identify definitions of the different levels of consequence relevant to the clinical area they are working in.
Once the risk levels have been identified, the risk can be rated using a matrix like the one below (recommended by the NPSA)
| Catastrophic | Yellow | Orange | Red | Red | Red |
| Major | Yellow | Orange | Orange | Red | Red |
| Moderate | Green | Yellow | Orange | Orange | Red |
| Minor | Green | Yellow | Yellow | Orange | Orange |
| Negligible | Green | Green | Green | Yellow | Yellow |
| Rare | Unlikely | Possible | Likely | Almost certain |
Clinical Risk Assessment
“The management of clinical risk to service users is a multidisciplinary process which should include the service-users and/or their carers. It involves making decisions based on knowledge of research evidence; knowledge of the individual service-user and their social context; knowledge of the service-user’s own experience; and clinical judgement.
All those concerned should collaborate in identifying potential clinical risks and the implementation of an agreed management plan to manage risks and make best use of the service-user’s own strengths to promote recovery. Risk management works best when a service user’s strengths are recognised alongside the possible problems that they might encounter and with which they might present.” NHS Litigation Authority (2012)
The Department of Health produced a document (2007) that described principles and evidence for best practice in the assessment and management of risk to self and others in mental health services.
This document outlines a framework for clinical risk assessment and management within mental health services, as well as describing the principle of positive risk taking.
It describes clinical risk assessment and management as “….a core component of mental healthcare…Effective care includes an awareness of a person’s overall needs, as well as an awareness of the degree of risk that they may present to themselves or others.”
The Department of Health identified 16 best practice points in relation to clinical risk assessment and management.
The first of these was: “Best practice involves making decisions based on knowledge of the research evidence, knowledge of the individual service-user and their social context, knowledge of the service-user’s own experience, and clinical judgement.”
Effective clinical risk assessment and management requires skilled staff. Staff should be trained in the skills and competencies required to conduct clinical risk assessments and the management of risk, including positive risk taking.
Management of risks
To service user
It is not usually possible to eliminate all risks but SLTs have a duty to protect patients/service-users as far as ‘reasonably practicable’.
This means you must avoid any unnecessary risk. All staff (both clinical and non-clinical) have a responsibility to contribute to the safety and welfare of service-users (DH, 2010).
The RCSLT suggest that practitioners:
- Work with other SLTs, professionals and services to ensure the safety and wellbeing of service-users.
- Assess and manage the identified risks involved in providing speech and language therapy services.
- Enable positive risks to be taken safely in cases where such risks are a necessary part of intervention and record the decision making (decision making tool, capacity assessment/links to decision making, decisions and signed off by MDT, service user, family).
- Develop, record and implement risk-management strategies to eliminate, avoid or reduce the likelihood of adverse events.
- Use incident/near-miss information to monitor and improve the safety of speech and language therapy services.
- Select and use equipment appropriately, providing adequate information and training on its safe use. (includes hygiene/infection control)
To practitioners
The RCSLT suggest that practitioners:
- Take reasonable care for their own health and safety.
- Inform the HCPC and their employer, if appropriate, about any health or personal conditions that may affect their ability to perform their job competently and safely.
- Limit or stop working if their performance/judgement is affected by their health.
- Refrain from any professional activities when under the influence of alcohol and/or drugs
An essential element to managing risks to the practitioner is effective use of clinical supervision and knowing when to seek help in managing a risky situation so that it doesn’t escalate.
As in all areas of practise, individual practitioners should seek help and/or advise if the situation is something beyond their experience or competence.
Health & safety/environmental risks
Any employer or organisation has obligations under the Health & Safety at Work etc. Act 1974 and all other Health & Safety Regulations to implement all reasonably practicable measures to reduce workplace risks.
RCSLT suggest that all practitioners:
- Abide by national and local health and safety regulations, policies and procedures within their own organisational context.
- Have a set of policies and procedures in place relating to the assessment and management of risk within their own organisational
- Take all reasonable steps to ensure health, safety and welfare of any person involved in any activity for which they are responsible.
Risk Management Strategies
Risk management strategies are actions required to reduce risks to an acceptable level.
It is often hard to judge the level of risk that can be tolerated. It is reasonable to accept a level of risk if the risk from all the other alternatives, including doing nothing, is even greater.
A risk is not acceptable if there is a reasonable alternative that offers the same benefit but avoids the risk. Acceptable risk may become unacceptable over time or because circumstances change. (NPSA)
Strategies identified to mitigate risks should be proportionate to the risk level. This means that the strategies chosen to manage any given risk should be appropriate / relevant to the likelihood and potential consequences of that event happening.
For example, an expensive or restrictive risk management strategy would not be an appropriate response to a risk that is assessed as unlikely to happen with only minor consequences if it did.
Risk management strategies may include (this is not an exhaustive list):
- Avoiding the risk One way to reduce risk is to stop doing whatever it is that creates the risk give example (for example, removing access to sharps bin from clinic room before paediatric clinic)
- Escalating the risk (with example)Informing senior managers with the authority and accountability to agree that they are willing to accept the risk on behalf of the organisation, or put necessary resources/controls in place to manage the risk. For example, informing senior managers of the risks to patients and the organisation of not being able to recruit to vacant speech and language therapy posts.
- Transferring the risk Risk transfer occurs when you get someone else to bear the risk for a particular activity. Examples include: Having a patient give informed consent to a dysphagia assessment or a videofluroscopy Taking out a warranty on new equipment that is purchased.
Controlling the risk Finding ways that you can reduce the likelihood of the risk occurring or of lessening the consequences of the risk. Some common strategies which can be used both to decrease the likelihood of risk, and lessen the consequences, include:
- ‘Where SLT assessment has indicated high risk associated with dysphagia or communication issues ensure that this assessment and management strategies have been communicated to key parties’
- Make sure that there are clear procedures in place for areas with identified high risks. These procedures might include what to do in the event of fire, procedures for dealing with hostile clients, aggressive individuals, procedures for when individuals have capacity to make unwise decisions etc.
- Clear procedures for following triage and prioritisation criteria in order to manage referrals and waiting lists.
- Provide adequate supervision for high risk areas. For example, where inexperienced staff are dealing with potentially aggressive clients, it is important that adequate supervision is provided
- Providing information – people need to know what to do if they are exposed to a risk. Consider “fire exit” signs, “warning” signs near hazardous materials and so forth. Information on how to use equipment and what to do in the event of accidents should be readily available.
- Provide training – the likelihood of risk will be greatly reduced when staff and volunteers have received proper training, for example in responding to challenging behaviours.
- Look for technological solutions – many risks can be reduced this way. Fire alarms and extinguishers, personal alarms, and burglar alarms each serve to lessen risks
Insuring against the risk
- For example, professional indemnity insurance
Accepting the risk
- A risk may be also accepted This decision may be made as part of a positive risk taking approach to working with individuals.
Guidance on specific situations
Lone Working
Working alone can bring risks to a work activity and the dangers of lone working cannot always be foreseen or avoided. Many potential incidents can be avoided and following relatively simple measures will significantly enhance staff safety.
Risk management strategies aim to reduce the likelihood, or impact, of a risk occurring. The list below are suggestions of strategies to manage risks associated with lone working.
Examples of strategies that may be effective, include: (this is not an exhaustive list)
- Carrying out regular supervisor or colleague checks during activities
- Using entrance security systems (i.e. digital locks or swipe cards)?
- Ensuring security lighting around access points and on-site parking areas
- Installing panic buttons linked to manned locations, and:
- Provide training to use them
- Regularly test them
- Ensure there are procedures in place to respond to any alarms raised
- Using two-way radio or other communication systems
- Practitioners being trained in conflict resolution and/or prevention and management of violence and aggression as appropriate to role
- Ensuring access to incident reporting forms and knowledge of how to complete these
- Individual client/visit risk assessments completed prior to each lone worker visit
- Practitioners being trained to complete a dynamic risk assessment when coming into contact with all members of the public
- Ensuring access to a telephone/outside line and are able to call for help in the event of an emergency throughout the working day
- Provision for accompanied visits when there are concerns about safety
- Including potential or known risk factors in referral documents and care plans
- Sharing risk information with other professional and agencies (e.g. police, social services and other healthcare trusts)
- Using systems for monitoring practitioners whereabouts and movements for regularly reporting to base
Part of the purpose of risk management by employers and SLTs is to develop safeguards, or alternative ways of delivering care, so SLTs do not feel that they would jeopardise their own safety in order to provide care for their patients / clients.
Ensure that you are familiar with your local lone working policy in order to reduce the risks associated with lone working.
Moving and Handling
Risk management strategies aim to reduce the likelihood, or impact, of a risk occurring. The following are suggestions of strategies to manage risks associated with moving and handling.
Examples of strategies that may be effective include: (please note that this is not an exhaustive list)
- All practitioners attending training in manual handling and/or back care
- A Movement and Handling Risk Assessment for all loads has been completed
- Where there are patient/client handling activities (including the use of restraint), the appropriate documentation been completed
- Copies of assessments being made available to all parties affected by them, either electronically or otherwise
- Suitable and sufficient mechanical aids available to help make patient handling and/or inanimate load handling safer
- Appropriate training has been provided for practitioners using movement and handling equipment
- All mechanical aids are in good working order and properly serviced and/or inspected where lifting equipment is being used
Violence and/or aggression
Risk management strategies aim to reduce the likelihood, or impact, of a risk occurring. The following are suggestions of strategies to manage risks associated with violence and aggression.
Examples of strategies that may be effective include: (please note that this is not an exhaustive list)
- The risk of violence to practitioners, service-users, visitors and contractors is assessed and precautions are put into place to minimise the risk
- All practitioners and visitors/contractors being made aware of these risks and the precautions to reduce the risks
- The strategies to reduce risk being consistent with current national legislation and guidelines including:
-
- The Health and Safety at Work etc. Act 1974
- The Management of Health and Safety at Work Regulations 1999
- NICE Guideline NG10 Violence and aggression: short-term management in mental health, health, and community settings
- Where a client has been clinically assessed as having a potential risk of violence, are practitioners are made aware of the control measures risk management strategies relating to that client
- Suitable support mechanisms being in place for any practitioner who is subjected to violence or abuse, e.g. referral to Welfare Officer, Staff Health etc.
- All incidents of violence resulting in injury are appropriately investigated and lessons learned are shared with all relevant people.
National Guidance
Please note: the resources on this page are provided for informational purposes only. No endorsement is expressed or implied, unless otherwise stated. While we make every effort to ensure this page is up to date and relevant, we cannot take responsibility for pages maintained by external providers.
- Many organisations will have their own Risk Assessment Forms but The Patient Safety Agency has produced a guide called Healthcare Risk Assessment Made Easy that explains the risk assessment process and has developed model forms that are provided on the National Patient Safety Agency’s website
- The Health & Safety Executive has also produced guidance regarding risk assessment which can be found at HSE – Risk Assessment – A Brief Guide to Controlling Risks in the Workplace and risk assessment templates are also provided on their website
- Depending on the risk being assessed, SLT’s may also have a role in supporting service user involvement in risk assessment, as well as integrating speech, language and communication needs of the patient in risk assessment and formulation for example, using an easier to read 5 p’s self-formulation with the patient
- Department of Health (2007) Best Practise in Managing Risk. Principles and evidence for best practise in the assessment and management of risk to self and others in mental health services
- National Patient Safety Agency (2007) Healthcare risk assessment made easy
- National Patient Safety Agency Guidance (2008) A Risk Matrix for Risk Managers
- Page, S (2010) Best Practices in Policies & Procedures
- Department of Health (2010) See, Think, Act
- NHS Litigation Authority (2012) An Organisation-wide Document for Clinical Risk Assessment and Management
- Control of Substances Hazardous to Health Regulations (COSHH)
- Flying Start (NHS Scotland) Web Pages (2018)
- Health & Safety Executive (2018) Managing Risks Well
- HSE Web Pages (2018)
Policy England
Here you will find links to relevant national legislation, policy and frameworks.
- Child Protection Act
- CQC standards
- Health & Safety Executive
- Mental Health Act
- Mental Capacity Act
- NHS Improvement – Patient Safety – National Reporting and Learning System
- The Care Act – Safeguarding Adults
- WHO Patient Safety
Please note that this list is not exhaustive. Please contact us with any suggestions.
Please note: the resources on this page are provided for informational purposes only. No endorsement is expressed or implied, unless otherwise stated. While we make every effort to ensure this page is up to date and relevant, we cannot take responsibility for pages maintained by external providers.
Policy Scotland
Here you will find links to relevant national legislation, policy and frameworks.
- Children (Scotland) Act 1995
- Children and Young People (Scotland) Act 2014
- Adoption and Children (Scotland) Act 2007
- Sexual offences (Scotland) Act 2009
- Limitation (Childhood Abuse) (Scotland) Act 2017
Please note that this list is not exhaustive. Please contact us with any suggestions.
Please note: the resources on this page are provided for informational purposes only. No endorsement is expressed or implied, unless otherwise stated. While we make every effort to ensure this page is up to date and relevant, we cannot take responsibility for pages maintained by external providers.
Policy Wales
Here you will find links to relevant national legislation, policy and frameworks.
- Children Act 1989
- Children Act 2004
- Children and Social Work Act 2017
- Adoption and Children Act 2002
- Children and Young Persons Act 2008
- Education Act 2011
Please note that this list is not exhaustive. Please contact us with any suggestions.
Please note: the resources on this page are provided for informational purposes only. No endorsement is expressed or implied, unless otherwise stated. While we make every effort to ensure this page is up to date and relevant, we cannot take responsibility for pages maintained by external providers.
Policy Northern Ireland
Here you will find links to relevant national legislation, policy and frameworks.
- The Children (Northern Ireland) Order 1995
- Children’s Services Co-operation Act (Northern Ireland) 2015
- Criminal Law Act (Northern Ireland) 1967
Please note that this list is not exhaustive. Please contact us with any suggestions.
Please note: the resources on this page are provided for informational purposes only. No endorsement is expressed or implied, unless otherwise stated. While we make every effort to ensure this page is up to date and relevant, we cannot take responsibility for pages maintained by external providers.
References
- Flying Start (NHS Scotland) Web Pages (2018)
- Health & Safety Executive (2018) Managing Risks Well
- HSE Web Pages (2018)
- National Patient Safety Agency Guidance (January 2008) A Risk Matrix for Risk Managers
- NHS Litigation Authority (2012) An Organisation-wide Document for Clinical Risk Assessment and Management
- Department of Health (2007) Best Practise in Managing Risk. Principles and evidence for best practise in the assessment and management of risk to self and others in mental health services
- National Patient Safety Agency (NPSA) (2007) Healthcare risk assessment made easy
- Page, S (2010) Best Practices in Policies & Procedures
- Department of Health (2010) See, Think, Act
- Department of Health (2007) Best Practise in Managing Risk. Principles and evidence for best practise in the assessment and management of risk to self and others in mental health services.


