Student placement case studies
As part of our campaign to address the shortage of placements for speech and language therapy students, we’re sharing case studies that demonstrate the benefits for both students and practice educators.
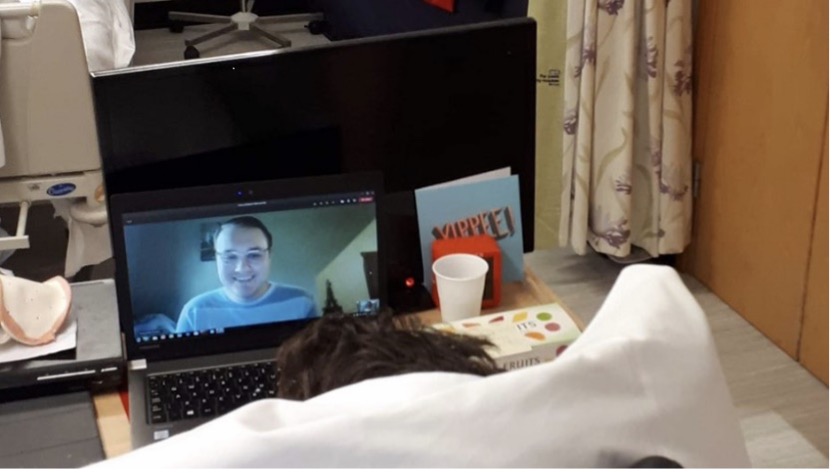
The added advantages of a virtual placement
Helen McDonald, a practice educator at Leeds Teaching Hospitals NHS Trust, and Joel Faucett, a second year student SLT, share their experiences of doing a virtual speech and language therapy placement via Microsoft Teams.
The practice educator perspective
Helen McDonald, practice educator, Leeds Teaching Hospitals NHS Trust
I contacted Leeds Beckett University (LBU) to see whether any student SLTs would be interested in volunteering via Microsoft Teams to provide some conversation practice and interaction opportunity to a young patient on the rehabilitation ward.
The patient had been in source isolation for a year following admission with a brain injury and due to the COVID-19 pandemic was no longer able to have visitors. The LBU placements team asked whether this opportunity could be turned into a placement to help an international student who was unable to return to the UK due to travel restrictions, and we gladly accepted the challenge!
The ‘virtual placement’ took place over three months, with sessions twice a week. These were carried out by the student and facilitated and observed by an SLT in the room with the patient. A weekly reflection, feedback and discussion session and some separate case study tutorials helped to inform the core skills assessment at the end of the placement. The student was also able to observe the patient in a physio session to gain experience of multidisciplinary (MDT) working.
As a first foray into the world of virtual placements, this experience allowed us to work out the best way to deliver a placement and get used to the technology required while only demanding a few hours a week of my time as a practice educator. This was especially important at a time when service demands were high and ever-changing due to the pandemic.
For the student, the placement provided consistent sessions over a few months, allowing him to really get to know the patient and see improvement. The twice-weekly sessions provided opportunities to demonstrate most of the core skills required, including rapport building, note writing, session planning, goal planning, reflection, and carrying out sessions independently. A few core skills were harder to assess, such as administering and interpreting assessments, but these were able to be signed off by using tutorials to discuss other cases.
For the patient, it was a really positive experience too – it allowed us to give him additional therapy sessions and provided a more ‘real’ communication situation/opportunity in which to practise speech strategies. It also gave him the chance to interact with someone his own age, at a time when his contact with the outside world was so limited.
I would encourage all placement educators to think outside the box when it comes to providing placements – you can find ways to enhance your service and patient experience by using students as part of your team.
Due to COVID-19, these kinds of opportunities are becoming more common – we should grab them with both hands because the benefits are clear for the student, the educator and the service user!
The student perspective
Joel Faucett, second year LBU MSc student
Last autumn, I had the privilege of undertaking a virtual placement with Leeds Teaching Hospitals speech and language therapy service. It involved working one-to-one with a client who had been isolated to a side room of a rehabilitation ward.
The goal of this placement was to provide the patient with the opportunity to practise conversation skills and serve as a form of social interaction in a time where hospitals were not allowing visitors due to the COVID-19 pandemic.
The placement lasted for roughly three months in total, consisting of bi-weekly sessions of 30 minutes to an hour, depending on the goals of the session and the patient’s MDT schedule. At the time of the placement, I was in the US and unable to return to England due to travel restrictions. Because of this, the placement was conducted entirely through Microsoft Teams with the assistance of a supervisor who would come in to set up the technology for the patient and assist if any technological issues arose. Fortunately, aside from the occasional WiFi glitch, there were no major technical problems – a wonderful achievement given the transatlantic nature of the placement!
Admittedly, I was initially skeptical about how much of an impact I could have working with a patient entirely online. I also worried that my learning would be limited under this arrangement. I am proud to say that neither of these concerns ever became an issue. Despite the virtual setting, I learned valuable clinical skills including strengthening session planning, functional goal writing and SMART target writing, the importance of establishing a strong rapport, and the value of patient-centred practice.
I also feel that this experience helped me to become a more adaptable clinician. Should a situation like the one we are currently in ever arise in the future, I feel confident knowing that virtual learning experiences can and do have a positive impact on both the student and patient. With the patient’s consent, I even got to observe a virtual physiotherapy session, and the physio team were excellent about answering any questions I had before and after their session with the patient.
Adjusting to the time difference was easily overcome by careful scheduling. Adapting to technology was also a challenge at first. But with time working out when to speak and how to use different screen share options for session activities got much easier and we made it work to the best of our abilities.
I would encourage students going on placement in any setting or situation to build a strong rapport with a patient. This can be achieved through active listening and tailoring session tasks to the patient’s personal interests. For example, the patient I worked with is a big football fan, so I tailored activities accordingly. For students who are embarking on a similar virtual placement opportunity, I would advise them to familiarise themselves with the technology as much as possible in advance of service delivery.
It was a great experience that I will always remember. I am so grateful to both Helen and LBU for providing me with this opportunity despite being nearly 6,000 miles away.
Students supporting quality improvement work
Susannah, a clinical lead SLT and practice educator, and student SLTs, Phoebe and Jen, discuss their experiences of a face-to-face placement on the Oxfordshire Stroke Rehabilitation Unit and share their tips for students going on placement.
The practice educator perspective
Susannah Stobart, clinical lead SLT and practice educator
In the autumn of 2020, I offered to deliver a weekly peer placement for fourth year students from the University of Reading, lasting 10 weeks. I work in the Oxfordshire Stroke Rehabilitation Unit, which is a 20-bed in-patient unit. We have been fortunate to be able to offer face-to-face placements throughout the COVID-19 pandemic.
The students were a pleasure to have on the unit. They demonstrated high levels of professional competence and settled into our multidisciplinary team (MDT) quickly. At the start I always challenge their placement goals to push them to achieve more. I also ask that they undertake a project for the ward. This year was brilliant. They produced a supported communication pack to assist capacity assessment around consent to care and treatment and created an aphasia friendly version of our patient leaflet. Both students presented their work to the ward staff.
The challenges were logistical. It was a full-time activity organising, discussing and reviewing patients, interactions and note writing. However, I learned that the buzz of peer placements works very well for me within our unit. While peer placements require careful planning, the rewards were great for both me and the ward.
Advice to students going on placement
- Help your practice educator (PE) to help you to achieve by having all the necessary paperwork to hand.
- Fill in your reports with the reflections you have made each week – this will help with discussion and evidence at mid-point and final report stages.
- Be prepared to stretch yourself from the start.
- Offer to do a project – this is good experience for you and helps your supervisor.
The student perspective
Phoebe Honey and Jen Tyldesley, student SLTs, University of Reading
We both completed projects and presented these to all the allied health professionals, healthcare assistants and nursing staff on the ward. This gave us the opportunity to work as part of an MDT and practise our presentation skills.
One thing we found most interesting was learning the skills to communicate with patients who had aphasia. Susannah, our practice educator, was incredibly supportive. She taught us so much and pushed us to achieve our potential. We got stuck in from day one and by the end of placement, we were planning and delivering therapy independently, as well as working with other members of the MDT.
Although we loved this placement, it had its challenges. Wards are busy places and can be demanding, so you need to think on your feet and be flexible. You are often working with patients who are quite ill and vulnerable and sometimes you need to have difficult conversations with patients. This can be emotionally challenging.
Our advice to new students on placement
- Really get involved with the placement. Throw yourself in at the deep-end and take any opportunities that come your way. The more you put into a placement, the more you will learn.
- Always have an open mind and be honest if you are struggling with something – don’t be afraid to ask for help.
- Most importantly, enjoy it, even if you have had to get up at 5am to get there!
We loved our time on placement and had an experience we will never forget. We can’t thank Susannah enough!
Download the Oxfordshire Stroke Rehabilitation Unit case study as a PDF
Adapting to placements during a pandemic
Ellen Baccino, 2nd year MSc student, Leeds Beckett University
I had the amazing opportunity to work in a community speech and language therapy team. The team covers two areas – long term condition management (LTCM) and stroke early supported discharge (ESD). The community SLT team can see patients who have a variety of different conditions such as motor neurone disease, Parkinson’s disease, multiple sclerosis (MS), respiratory conditions such as COPD (chronic obstructive pulmonary disease), dementia, stroke (after ESD) and generally frail and elderly patients, with associated swallowing and/or communication disorders. The team also sees adults with learning disabilities where their main difficulty is thought to be as a result of one of the conditions above.
I was able to observe my placement educator supporting dysphagia patients in care homes via telehealth. I mainly worked independently with two patients for my eight-week placement – Patient A, with a diagnosis of multiple sclerosis and mild dysarthria characterised by reduced volume and variable imprecise articulation, and patient B who had experienced an acute left total anterior circulatory stroke and as a result, had moderate receptive and expressive aphasia.
With Patient A, I carried out a six-week in-house Loud Programme via Microsoft Teams to improve vocal loudness, practice variation in pitch, articulation and intelligibility. I learned a lot from this experience as I carried out the programme independently each week which I had never done before. I also researched further interventions and adapted them into the programme to ensure I remained patient centred. It really boosted my confidence to hear Patient A’s positive feedback about my sessions.
I really enjoyed creating resource sheets to support the patient to continue to use the strategies learned in therapy in daily life, as I could combine patient support with creativity. The challenges were that sometimes we experienced technical difficulties. This meant we had to re-arrange our session or revisit areas, so it was important to remain professional, flexible and adaptable.
With Patient B, I carried out independent home visits during the COVID-19 pandemic and I had to wear PPE. Before each visit, I would conduct a telephone COVID-19 risk screen. I created a care plan and session plans for each week, which I ensured were engaging and motivating for the patient. I worked with the patient on different aspects of language such as comprehension and expression, reading and writing skills by creating tailored language activities. It was wonderful to see Patient B’s progress over a short period of time. The patient had improved in her comprehension and expressive skills over the course of two months of speech therapy input in comparison to baseline measurements.
My advice to future students going out on placement would be to make the most of every opportunity, put as much effort in as you possibly can as the more you put in the more you will get out of the experience. Ask questions as and when they arise and remember wherever you are challenged, you are equally supported.
Learning from a virtual placement
Philippa Bowen, specialist SLT, community paediatrics, Chesterfield Royal Hospital NHS Trust
We were faced with the challenge of providing a final placement for second-year master’s students in the middle of being plunged into a teletherapy world. As always, our main priorities were for the placement to be as beneficial as possible for all parties involved. Since there were three therapists sharing the placement we tried to offer as varied an experience as possible by combining remote therapy sessions with producing a number of therapy videos aimed at parents.
I took on responsibility for supporting the student in producing several short videos to accompany the speech programmes that we use in the department. The end product would reflect the students:
- Understanding of the therapy approach (what and why)
- Delivery of information in a clear and appropriate way for the audience (who)
- Organisation and planning skills (how)
- Ability to reflect and refine the information and presentation.
It was helpful for me to have experience of making similar videos myself, particularly so that I was aware of the process and potential pitfalls.
It quickly became apparent that the success of this project relied upon a significant amount of revision and research on behalf of the student. The placement consisted of regular support sessions for:
- Revising the therapy area (speech sound therapy, silent sorting)
- Critiquing similar videos that were freely available on YouTube
- Formulating a session plan (not dissimilar to a therapy plan) where the key was to keep it short and simple.
- Producing the video that the student happy with in terms of presentation and message
We estimated that this process took 8 hours of placement time per video.
As it turned out, the student was then able to use 1 of the videos (silent sorting) in a remote therapy session and to send it to the parent for future reference.
As a therapist, this remote placement was an interesting and manageable way to provide a supported student experience, while fulfilling the placement requirements.
Feedback from the student was extremely positive. It was a challenging and memorable learning experience, which combined learning new skills with consolidating developing therapy knowledge and techniques. There was also a requirement for extensive revision and reflection.
As a practice educator with many years of experience, I will now be incorporating the production of therapy videos in future placements as a useful learning experience and consolidation of skills.
The benefits of a blended placement
Ceri Read, 2nd year MSc student, City University, London
I recently completed a placement in West Sussex with the early Years Clinic Team, 2 days a week for 5 weeks. I learned all about speech sound assessment and therapy. I learned how to create activities to facilitate speech sounds therapy through PowerPoints shared via teletherapy. I also had the opportunity to observe their autism diagnostic service.
I really enjoyed observing the role of SLT in diagnosing autistic spectrum conditions (ASC). I also found it interesting to observe the impact of the pandemic on the service. I learned when switching to face to face sessions was essential, either due to unreliable technology or being unable to determine whether a child is making a sound or not. I also found it fascinating to see how teletherapy had expanded service delivery since children who previously would have been unable to attend the clinic were now able to access SLT.
The placement gave a mixture of teletherapy and face-to-face experience since all teletherapy sessions were completed in the office with my practice educator. The team was so welcoming and accommodating which made the experience much richer. I learned a lot from sitting in on team supervision sessions and informal discussions in between sessions in the office. This gave me a more holistic view of how the service worked. This also gave me an insight into where I would like to work when I qualify.
Reflections on hosting a student placement
Abigail Scott, practice educator and SLT, Wiltshire Children’s Community Services
Hosting a student placement is always rewarding but hosting a community paediatric placement during a pandemic meant adapting to a range of different challenges. Our year 4 student was with us for three days a week from September to November 2020 and joined us in offering virtual and face-to-face appointments to children aged 2 to 16. She was a great asset to the team.
Benefits of having a student
Our student was keen to develop her skills and quickly managed several cases with support, which was a welcome help with a large caseload. She had a very positive impact on the lives of the children she worked with. We continue to use the resources she created, and we valued her ideas for fun games and approaches.
Exploring new resources and findings from her studies helped us to reflect further on and develop our practice.
Therapist learning
Therapists were able to develop their supervision skills, eg their abilities to explain the rationale behind clinical decisions and support the student to self-reflect on sessions.
Challenges
It was very difficult to give the student a plan for what the days would look like in advance due to the increased need for working flexibly during the pandemic.
It was a challenge balancing supporting the student with a range of other demands such as managing large caseloads of children with a high level of need. This meant that we couldn’t always offer support in the most ideal way for the student. For example, we found it less effective to provide feedback via virtual conversations and felt this would have been easier if we had been able to meet face-to-face more frequently.
At times, the student needed support to be realistic about what onward referrals were appropriate at what points in a child and family’s journey. We supported her to feel comfortable with the learning process, reflecting on what she’d done well and what she would do differently next time.
Advice for students going on placement
- Remember that every placement is different.
- Be flexible – children are unpredictable!
- It’s OK to make mistakes – it is how we learn.
- Your clinical educators don’t expect you to know everything – you are on placement to further develop your knowledge and skills.
- Be mindful that progress can take time for some children – celebrate successes with parents/ supporting adults.
- Learn to write simply and summarise – notes and reports need to be understood by everyone. Think about the important messages you want to record and share with the child’s team.
- Be open to all feedback. Your clinical educator’s role is to support you and help you to grow as a therapist.
Learning from the hyper acute stroke unit
Pippa Moore, 2nd year MSc student, UCL
PPE (Positive Placement Experience)
I have been reflecting on my recent placement on the Hyper Acute Stroke Unit (HASU) at Queen’s Hospital in Romford. Every Monday since October I have had the slightly surreal experience of arriving at the staff entrance to the hospital, with a slight spring of imposter syndrome in my step as I flash my ID badge, put on my scrubs, swap my surgical mask for a fresh one, take my temperature and sanitise my hands for the first time that day. Only recently have I learned to navigate my way around the vast, maze-like hospital with its seemingly hundreds of staircases and lifts. But finally, in my last few weeks, it began to feel like somewhere I belonged.
Having had 2 of 3 first-year placements cancelled when the pandemic first broke out, I was both relieved and apprehensive to find out my second ever placement would be in an acute setting. Hospitals can be a sensory overload at the best of times, and I was expecting this to be heightened during the peak of the second wave. But much to my surprise there was an eerie calm about Queen’s, with no families visiting, empty corridors, social distancing, and a noticeable absence of the general chatter of staff scoffing their lunch down in the cafeteria as they share stories during their half-hour break.
I have always wanted to work with people with acquired disorders, and I am grateful this placement allows me to see a person’s journey from the very start of acquisition, when they are at their most vulnerable. I quickly learned the importance of early intervention with stroke patients. New admissions and those ready for discharge are prioritised for communication assessments, before attending to those identified in their initial screening as having acquired communication deficits. This makes for a sophisticated caseload prioritisation MDT meeting each morning with SLTs, occupational therapists and physios (think ‘episode of Casualty with loads of medical terms flying about’).
Now that I have got to grips with the comings and goings of a stroke ward, I am feeling more confident to leave the very safe and comfortable nest of my practice educator to do things independently. Finally, I am able to start fulfilling the reason I chose to embark on my journey to become a SLT – to help people to communicate when they are most in need. To give people the time and patience they deserve. To live up to the ‘everyone deserves a voice’ logo on my hospital tote bag.
My advice to students feeling apprehensive about placements – You will make mistakes. But you will learn from them and come back better equipped to tackle future challenges, and ultimately, become the best SLT you can be.
A virtual training placement
Dominic Carroll, Phillipa Cooke and Holly Standish, final year BSc students, Leeds Beckett University
As three final year students, we collaborated to prepare and present virtual speech, language and communication needs training via Microsoft Teams recordings and pre-recorded video, to teaching assistants in a mainstream school, over a period of eight weeks. The training sessions aimed to provide a foundation of knowledge in speech, language, social communication, selective mutism and stammering.
We learnt how to work remotely as a group and prepare and record Teams presentations. We also learnt how to pre-record, edit videos and upload them to SharePoint for other users. Delivering to a camera, where errors can be re-watched or kept for perpetuity, can be intimidating. But condensing three years’ worth of learning into five 45-minute sessions with accompanying PowerPoints was a valuable experience for clarifying what we had studied. It was also really beneficial to work alongside education professionals. We were able to administer assessments, set targets and then offer therapy sessions. Our clinical knowledge has improved as we put theory into practice – learning how to train education professionals was an invaluable experience.
We worked out how to deliver complex information in an accessible fashion, what was necessary (and interesting) for the audience to know and finding ways to present these with accompanying visuals. It was a good working environment once we got into the flow of the project. We delivered different sections of the training week-by-week, checking in with each other, our educator, and the staff at the school.
We came up with creative ways to boost staff engagement and interaction. As a group, we added small reflection tasks, videos, or interactive elements to the presentations. Initially there were tech challenges, such as getting used to SharePoint and multiple Teams accounts. Additionally, wifi and laptop problems often meant dropped calls and documents failing to load, but overall it was a great learning experience.
Our advice for students going on a similar placement:
- Take time to front-load a lot of the pre-project organisation and planning and appreciate how much this organisation is a valuable part of the project. This involves familiarising yourself with new technology or software, setting up a plan for how you will share and approach the work, and how and when you will approach admin and scheduling.
- Make the most of software available to you, such as Microsoft To Do lists or Teams calendars.
- Get used to scheduling in your time formally with tools that work for you (and remember that scheduling your week also takes up time in your schedule!)
- Be realistic about how much time you are going to give to the project – when you are working at home on university studies, it is very easy to slip into working at home on placement projects as well.
- Have a plan for what you will do when things go wrong or when you have wifi problems and take it in your stride. These things will happen, so maintain a friendly, professional attitude when they do.
- Keep anonymised copies of the materials and feedback for your standards of proficiency portfolio.
Growth opportunities from an ‘out of comfort zone’ placement
Nessa Stringer discusses what she’s learnt from her speech and language therapy placement at a medium-secure forensic psychiatric unit.
Nessa Stringer, 2nd year BSc student, Canterbury Christchurch University, @Speechie_Ness
I am just over halfway through a 12-week placement at a medium-secure forensic psychiatric unit. Patients are detained under the Mental Health Act and all have a mental health diagnosis. They have all had contact with the legal system but are often too unwell to be detained in prison settings, which is why they are detained in these types of forensic units. Being a medium-secure setting many patients have very complex, and often traumatic, histories.
My placement is mainly virtual, so I join sessions via Skype. This brings its own challenges. For many patients in forensic settings, trust is often something that has been irreparably broken in their lives; therefore, it is hard for these individuals to build trust with their regular speech and language therapist (SLT), let alone with a student on a short-term virtual placement.
Something I find challenging are the occasions where patients decide, often at the very last moment, that they didn’t feel happy to consent to me joining the sessions remotely. What I have learnt is it’s not about the SLT or the student. It’s about your patient/client and remembering that they are at the centre of all you do. So, I will take that and build on it.
The advice I would give to other students about to go on placements, especially to settings they had not expected to go to, would be to just say yes! Take the opportunity for growth, get out of your comfort zone and be open-minded. These are the situations where you will learn the most both professionally and personally.
It’s also important to remember not to be afraid to ask questions, even in multidisciplinary team (MDT) meetings. We’re still learning so no one is expecting you to know all the answers and make all the right deductions.
I have a wonderful practice educator who is always supportive and encouraging. She has taught me to always be mindful of ways to involve my patients, to ensure they have autonomy with their therapy sessions.
A practice educator’s perspective of a virtual placement
Alison Matthews, SLT, Elysium Healthcare and Total Communication Services CIC
I recently hosted six first year students from the University of Manchester on a virtual placement for three weeks. The placement was based with Elysium Health Care and included sessions with my community interest company, Total Communication Services CIC.
Two of the students were based internationally which involved some time differences and challenges. We focused the placement on the provision of accessible information. I provided a day’s training and gave them projects to work on in pairs.
The students produced some high-quality information which would have been time consuming for me to create. Their interest and passion was a real tonic at times given the challenges of lockdown. They had time to read around topics, research the area and consider available resources.
I facilitated opportunities for the students to connect with service users virtually. I asked one patient at the hospital to teach them his speech and language therapy programme we have been working on for dysarthria. The students had just had lectures on this topic, and they were delighted to interact with him and ask questions. I did not want him to feel like he was in a virtual goldfish bowl with six people peering at him from the screen, so shifting the power and making him the teacher was a positive experience all round. By the end of the session, he had adopted the style of a talk show host and asked if they wanted to ask any further questions before he left.
Although there were challenges with time keeping and managing a group of people virtually, we set up a WhatsApp group so we could maintain prompt communication.
My advice to students embarking on a placement:
- Treat the placement as 9am–5pm every day unless you are told differently.
- Treat it as if you are in paid employment – if you need to be absent ask permission, don’t just assume you can make up the time later.
- Try to remain focused and engaged in online sessions. These are hard for everyone and practice educators need to know that they are making sense!
- Check whether you can send in drafts of work for comments, and if so, when. You can use this for feedback.
- Use the online reflection system – it’s a much easier way of the practice educator understanding how you are thinking and the stage of your clinical development.
- Read around subjects while you have the time.
- Offer feedback when asked.
- Work as a group and support each other.


