What is enhanced practice?
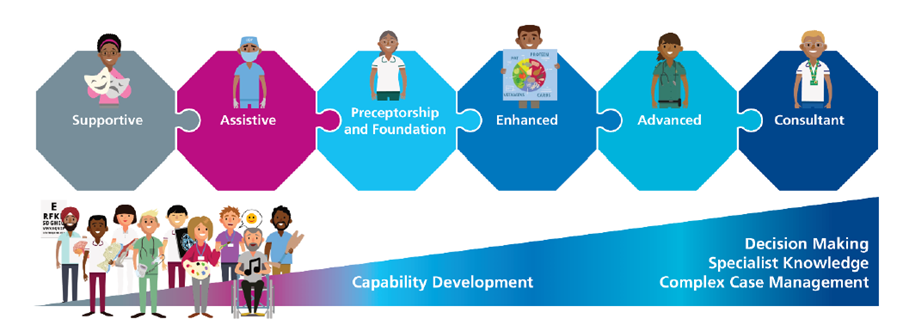
Enhanced level is defined as having an in-depth knowledge and understanding of an area of practice and routinely delivering a high standard of practice. Enhanced practice is a level of practice healthcare professionals can attain and is used to describe the practice of highly experienced, knowledgeable healthcare professionals.
Completing an enhanced practice course would cover all four pillars, including research, education, leadership and clinical practice. The research, education and leadership aspects would generally be less specific and more focused on multi-professional working. The clinical aspect would be profession specific, enabling a clinician to become more confident and enhance such skills.
The current routes to reaching this level of practice include CPD and completion of a level 7 Enhanced Practice Apprenticeship (please note, RCSLT are working on the development of these courses, they are not available to SLTs yet). Completion of a course does not create the job title ‘Enhanced Practitioner’. This is a level of practice rather than a job title. There is likely to be a variety of different job titles once enhanced level is reached, these may include ‘Community specialist’, ‘Extended Scope Practitioner’ or ‘Specialist frailty SLT’.
Enhanced Practice is not targeted for new qualified practitioners. Although timeframes are not exact, we would expect a clinician to focus on NQP competencies and potentially their preceptorship before considering enhanced practice. Therefore, someone may look at enhanced practice roughly 18 months after their preceptorship. In general, enhanced practice would be for band 6 clinicians if working in the NHS. The competencies can be recognised and followed by familiarising yourself with the ‘enhanced’ section of the Professional Development Framework.
RCSLT are actively working on developing Enhance Practice opportunities for SLTs. For more information, please contact Will at William.christopher@rcslt.org.
Purpose and benefits
The purpose of enhanced practice is to:
- Maximise professional capabilities to ensure services are safe and productive – quality assurance
- Encourage retention of staff by providing clear career progression pathways
- Offers CPD and career progression opportunities e.g. leadership
- Support standardisation of workforce strategy
- Meet service demands
- Manage a discrete aspect of a patient’s care within their current level of practice, which will be particular to a specific context
- It is not expected to replace existing educational pathways
Benefits to the clinician and employer include:
- Clear pathways for career progression
- Supports the clinician to enhance their skills and increase confidence
- Helps to prepare clinicians for advancing further into their career
- Provides the service with more highly trained clinicians who are prepared and understand MDT working
- Provides the service with more highly trained clinicians, hopefully enabling wait times to be shortened and utilises the enhanced skill set of the clinicians
The enhanced practice apprenticeship
The Enhanced Practice Apprenticeship was developed by the Institute of Apprenticeships and would require attendance on the course one day a week over 18 months, the remaining 80% would be employer led. Read more about the apprenticeship standards.
The final certificate is a 60 credit PGCert. The apprenticeship levy offers £7,000 for anyone completing the course. Find out more information about how the levy works.
Enhanced practice and advanced practice
There has been some confusion with how enhanced practice interacts with advanced practice. Enhanced Practice may be the target destination for some clinicians but it also acts as good preparation for those who may want to become an AP or consultant. If someone did want to move onto advanced practice, there would be the expectation to remain at the enhanced practice level for around 5 years, encouraging growth in both profession specific knowledge but also the dynamics of multidisciplinary working.
Advancing practice is an advanced level of practice in which a practitioner has demonstrated their ability to work at a high level including clinical duties, leadership, education and research. They would be expected to be a leader, educator, highly skilled clinician and have an understanding of the wider health and care system. Find out more about advancing practice.
Here are some of the key difference between enhanced level of practice and advanced:
| Enhanced practice | Advanced practice |
| Manages risk but defers major decision making | Manages risk |
| Uses freedom to act within own scope of practice | Uses freedom to act, and provides professional leadership and supervision in situations that are complex and unpredictable |
| Has a specific body of knowledge | Has a highly developed specific body of knowledge |
| Uses complex decision making but confers with others for overall plan | Uses a high level of complex clinical decision making, including complete management of episodes of care |
| Often manages a caseload, sometimes providing interventions as part of a dedicated clinical pathway | Manages defined episodes of clinical care independently from beginning to end |
| Post registration qualification/ CPD and occasionally masters qualification | Masters level |
| Will work with national and local protocols where these exist | Will shape the design and delivery of local protocols where these exist |