Head and neck cancer – overview
Key points
- Head and neck cancer occurs mainly in adults, however, some children may present with either benign or malignant tumours of the head and neck
- Speech and Language Therapists (SLTs) develop and support the communication skills of both the patient and communicative partners
- SLTs have a unique and essential role to help facilitate alaryngeal voice restoration post laryngectomy
Introduction
This information is for anyone who would like to find out how speech and language therapists (SLTs) work with people with head and neck cancer. You may have been diagnosed with head and neck cancer or know someone who has. You may want to find out more about what speech and language therapists do and how we can help. If you’re a speech and language therapist, please sign up or log in to access the full version of this guidance.
Having head and neck cancer and its treatment can affect your eating, swallowing and communication.
SLTs support people before, during and after treatment. SLTs working with people with head and neck cancer may help you by:
- sharing information about possible changes in talking and swallowing
- assessing swallow, voice and communication and listening to any concerns you are having with these
- giving advice and exercises to help make eating, drinking, swallowing, mouth opening and talking as good as it can be before, during and after treatment.
Treatments for head and neck cancer can have long-term side effects and people may need the support of SLTs again, sometimes years after their first treatment.
SLTs work closely with other health professionals supporting people with head and neck cancer e.g. dietitians, head and neck nurse specialists or surgeons. They will listen to you and what is important to you before planning treatments or recovery goals. Head and Neck SLTs work in different settings (including outpatient clinics, hospital wards, people’s homes and hospices) and work closely with other professionals to support people at all stages of head and neck cancer treatment and care.
What is head and neck cancer?
Most types of head and neck cancers affect the lining of the mouth and throat. The lymph glands of the neck may also be involved. When a cancer is diagnosed, tests are done to find out the size of the tumour and if it has spread from its original location into lymph nodes. More information on head and neck cancer, including different types, staging and grading is on the Macmillan website.
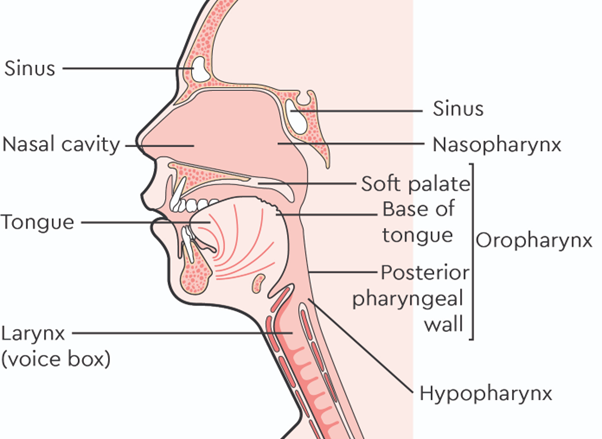
Head and neck cancers include cancers of the:
- mouth (oral cavity): including lips, inside of the cheeks, gums, floor of mouth, roof of mouth or the front of tongue
- nasopharynx: the upper part of the throat behind the nose
- oropharynx: the part of the throat at the back of the mouth, includes the base of the tongue and tonsils
- hypopharynx: the lower part of the throat connecting the food pipe (oesophagus) and windpipe (trachea)
- voice box (larynx)
- nasal cavity and sinuses
- salivary glands (parotid, submandibular and sublingual)
Other cancers such as thyroid, certain tracheal or lower oesophageal cancers are not called ‘head and neck cancers’. However, as these cancers are so near to parts of the head and neck used for swallowing or voice, people with thyroid, tracheal or oesophageal cancers may still be seen by a SLT. Head and neck cancer occurs mainly in adults; however, some children can have it too.
This YouTube video produced by Cancer Research UK explains where different parts of the head and neck are.
Head and Neck Cancer Statistics
- Around 12,400 new cases of head and neck cancer are diagnosed in the UK each year, which is 34 people diagnosed every day. This is expected to be 16,300 cases a year by 2038-2040.
- The above statistics are from July 2023; for the most up to date statistics on head and neck cancer, see Cancer Research UK.
Reducing the risk of developing head and neck cancer
When someone has head and neck cancer the exact causes are likely to be unknown. However, it is possible to lower the risk of head and neck cancers e.g. by getting help with stopping smoking, drinking less alcohol or improving diet. See the Macmillan website for further information on risk factors. An increasing number of head and neck cancers, especially at the back of tongue, throat and tonsils, are linked to infection with human papillomavirus (HPV). See the Mouthcancer Foundation leaflet for more information on HPV. The HPV vaccination programme is likely to reduce the number of HPV-related cancers over time.
Symptoms of head and neck cancer
Contact your GP if you have a neck lump, mouth ulcer, pain in the throat or mouth, painful swallowing, difficulty swallowing or voice changes for longer than three weeks. See the NHS website for more symptoms of head and neck cancer.
Treatment for head and neck cancer and side effects
Treatments for head and neck cancers include surgery, radiotherapy, chemoradiotherapy, targeted therapies or immunotherapies, these are explained on the Macmillan website. People may need more than one type of treatment to treat or control the cancer.
People with head and neck cancer often have changes to their speech, voice and swallowing as a result of the cancer or its treatments. Some people may also have changes to breathing, smell and taste. It may be hard to talk, eat or drink with others or return to work. This can have an impact on people’s wellbeing, social life and work.
Up to 75% of head and neck cancer patients have swallowing problems at diagnosis (Patterson et al, 2013, Russi et al, 2012), and 60-75% after treatment (Malagelada et al, 2015). Eating and drinking problems can cause chest infections, pneumonia, needing to use feeding tubes or weight loss. Swallowing problems can cause embarrassment, anxiety and avoiding eating with others. Difficulties with communication can make it harder for you to talk with other people which can lead to feeling isolated, depressed and lonely. Without support, these difficulties can also affect your ability to return to work or join in with other daily activities.
How can your speech and language therapist help you?
SLTs support people with head and neck cancer throughout their treatment journey. They work alongside the healthcare team to support individuals and their families to make choices about their treatment and recovery goals. SLT input may still be needed many years after the original treatment to help if you are having long term side effects of treatment.
SLTs can support you in the following ways:
- SLTs support people with head and neck cancer and their families before, during and after treatment.
- Can work with you on eating, drinking and swallowing –
- e.g. making changes to drinks or food
- or helping you to swallow more easily and enjoy eating and drinking
- or finding ways to help stop things going down the wrong way when you swallow (if this is a problem for you). This could be a head position or technique to use when swallowing to help food or drink to go down the right way.
- Please see our RCSLT factsheet to find out more about how SLTs support people with swallowing difficulties following head and neck cancer.
- perform specialist swallowing assessments –
- e.g. a video x-ray of swallowing called videofluoroscopy or using a flexible camera passed through the nose to look into the throat and assess swallowing. This is called fibreoptic endoscopic evaluation of swallowing (FEES)
- check if someone is able to swallow, cough, use their voice and clear their saliva properly –
- e.g. SLT assessments help hospital teams to decide whether a person’s temporary breathing tube (tracheostomy tube) is ready to be removed after head and neck surgery. Not everyone needs a temporary breathing tube after head and neck surgery.
- help decide whether someone is able to meet their food and drink needs by mouth, if they may need help from a feeding tube or food or drink with extra nutrition. The SLT will work closely with the person being assessed, dietitians and the rest of the healthcare team to reach these kinds of decisions.
- give clear recommendations of safest food textures or drink thickness based on the International Dysphagia Diet Standardisation Initiative (IDDSI) framework – SLTs use the same ways of describing food and drink internationally.
- SLTs can support you in ways of communicating –
- e.g. giving voice therapy after radiotherapy if your voice has been affected
- or helping you if you have had removal of the voice box (total laryngectomy) to learn different ways to produce voice
- or helping you to record your own voice (voice banking) before treatment for use after treatment. If your treatment is likely to significantly change your voice after treatment, SLTs can offer more information about this (if available in your local area) or provide support looking at options for this.
- make rehabilitation programmes –
- e.g. help you to use equipment and do exercises which will help with swallowing, speech, voice, breathing or mouth opening
- or give you exercises for the swallowing muscles to do before, during and after radiotherapy or surgery
- help breathing and better lung health after surgery for people who breathe through a hole and / or a breathing tube in their neck e.g. after laryngectomy surgery, or people with a tracheostomy tube.
- e.g. recommending products which can filter and moisten the air you breathe in, in a similar way to what the nose would normally do when breathing in
- if your treatment will include having your voice box (larynx) removed (total laryngectomy), SLTs will help you to use new ways of having a voice and to make communication easier. SLTs can also help with breathing, taste, smell and swallowing changes after total laryngectomy –
- e.g. recommending products which can filter and moisten the air you breathe in, in a similar way to what the nose would normally do when breathing in
- can help you to meet others who have already had similar types of head and neck surgery (which can change speech, breathing, swallowing or appearance) –
- e.g. arranging for you to talk to someone who has already had the operation before having total laryngectomy (removal of the voice box) or total glossectomy (removal of most of the tongue) surgery
- give information and support for people living with and beyond head and neck cancer treatment –
- e.g. putting you in touch with local and national cancer support groups and centres or other professionals (such as head and neck clinical nurse specialists or clinical psychology services) or online resources and patient conferences
- help to improve swallowing and communication for head and neck cancer patients by being involved in research and ways to make services or treatments better.
Useful links to online resources for head and neck cancer
You may find some of the following online resources useful. They are listed alphabetically. RCSLT does not accept any responsibility for the content, or updates of these websites and documents or endorse any products mentioned in these resources. There may also be useful laryngectomy information on the websites or YouTube videos of companies who produce laryngectomy products, but as these promote certain products, they have not been included here.
- Cancer Research UK: A good source of statistics regarding cancer and information on the latest research including clinical trials open in the UK, cancer chat forum and nurse helpline, information on to how to find a counsellor, and advice on how to support someone with cancer.
- Get ahead Charitable Trust: Supporting those with head and neck cancer through education, treatment and research.
- Get checked early: An online symptom checker, patient stories and information on head and neck cancer and what to do if you are worried about symptoms in yourself or others.
- Head and Neck Cancer UK: Acts as an advocate for head and neck cancer patients and their families and provides information and advice on head and neck cancer including details of local support organisations.
- Head and Neck Cancer Coalition UK: A group of 15 organisations working together to provide research, patient and carer support, change policy, improve services and increase awareness and education into head and neck cancer.
- Macmillan Cancer Support: Provides useful information to support people with head and neck cancer and their families including details of symptoms, diagnosis, grading and stages of head and neck cancer and treatment options, online booklets in different languages, online support 24 hours a day, cancer forums and a helpline. Macmillan have a YouTube channel with videos on understanding cancer, personal stories and living with cancer. They have produced a video about speech therapy and voice restoration after cancer.
- Heads2gether: An in person and virtual support meetings for patients and caregivers.
- Maggie’s: Provides online support regarding managing emotions, social and practical help e.g. with finances, managing symptoms and side effects and supporting someone with cancer. Maggie’s Centres are specialist buildings across the UK with support specialists, psychologists, benefits advisors running drop-ins, support groups, courses and workshops for people affected by cancer.
- Marie Curie: Information and support for people diagnosed with terminal illness.
- Mouth Cancer Foundation: Raises awareness of mouth cancer through free information materials (available in different languages) provided to healthcare professionals, patients, carers and the general public, online patient and carers community forum and helpline, have produced a cookbook for people who have difficulty chewing or swallowing food.
- National Association of Laryngectomee Clubs: Gives support for people with laryngectomy including information packs, online leaflets, a telephone helpline, newsletter, online meetings, local support groups, advocacy for people with laryngectomy and involvement with research projects. They have a YouTube channel of videos and resources and over 60 affiliated laryngectomy clubs.
- National Tracheostomy Safety Project: Information and resources about tracheostomy or laryngectomy for patients, carers and for healthcare professionals to improve patient safety and care. They have a YouTube channel of their videos.
- NHS website – head and neck cancer section: Head and neck cancer statistics, different types of head and neck cancer and links to further reliable sources of information. NHS Greater Glasgow and Clyde have produced a video on ‘Care of Laryngectomy’.
- Oracle Cancer Trust: Supports programmes and funds research into head and neck cancer
- Relay UK: A service which can be set up for people to text 999 in case of an emergency, which can be useful for people unable to speak clearly on the phone.
- Salivary Gland Cancer UK: A charity for those with rare salivary gland cancers. Support all patients, caregivers and clinicians treating rare salivary gland cancers. Holds regular hybrid gatherings to provide peer support, reliable information and opportunities to further research.
- Sarcoma UK: Funding research and offering support for anyone affected by sarcoma cancer and campaigns for better treatments, Sarcoma UK is the only cancer charity in the UK focusing on all types of sarcoma.
- Saving Faces: The Facial Surgery Research Foundation: Provides online information on surgical procedures, has a patient helpline and can put people in touch with people who have had facial surgery or changes in appearance due to treatment for support. Saving Faces is also involved in education and research to improve physical and psychological treatment for people with oral cancer.
- Shout at Cancer: A charity specialising in speech training with music after laryngectomy, including breathing, singing, acting and beatbox exercises.
- The Sunderland Cookbook Project: A cookbook by and for head and neck cancer patients to discover ways of enjoying food again, South Tyneside and Sunderland NHS Foundation Trust and the University of Sunderland.
- The Swallows Head and Neck Cancer Group: A 24/7 support line, monthly patient, caregiver and family members meetings (including virtual), organises international conferences for patients, carers and healthcare professionals. Has links to research projects to get involved with on the website.
- Throat Cancer Foundation: Hosts a patient and cancer forum, information on throat cancer, treatment and care. They campaign for a ‘Gold Standard of Care’ for patients and improving post-treatment quality of life and are also involved with research.
- Young Tongues: An international peer to peer support group made up of young people who have been diagnosed with Tongue Cancer or a cancer diagnosis that involves similar treatment. They connect via chat groups, virtual meet ups and social media and podcasts.
Other references:
- Malagelada, J., Bazzoli, F., Boeckxstaens, G., De Looze, D., Fried, M., Kahrilas, P., Lindberg, G., Malfertheiner, P., Salis, G., Sharma, P., Sifrim, D., Vakil, N. and Le Mair, A. (2015). World gastroenterology organisation global guidelines: dysphagia-global guidelines and cascades update September 2014. J Clin Gastroenterol. 49(5), 370-8.
- Patterson, J., McColl, E., Carding, P., Hildreth, A., Kelly, C. and Wilson, J. (2013) Swallowing in the first year after chemotherapy for head and neck cancer: Clinician- and patient-reported measures. Head Neck, 36 (3), 352-358.
- Russi, E., Corvò, R., Merlotti, A., Alterio, D., Franco, P., Pergolizzi, S., De Sanctis, V., Ruo Redda, M., Ricardi, U., Paiar, F., Bonomo, P., Merlano, M., Zurlo, V., Chiesa, F., Sanguineti, G. and Bernier, J. (2012). Swallowing dysfunction in head and neck cancer patients treated by radiotherapy: review and recommendations of the supportive task group of the Italian Association of Radiation Oncology. Cancer Treat Rev, 38(8), 1033-1049.
Contributors
We are grateful to the author group, the project reference group and all those who contributed to the development of this guidance.
Lead Author
Ceri Robertson
Supporting Authors
Dr Margaret Coffey
Nicky Gilbody
Dr Roganie Govender
Rhiannon Haag
Claire Hooper
Kirsty McLachlan
Professor Jo Patterson
Diane Sellstrom
Freya Sparks
 Download as PDF
Download as PDF

