What is advancing practice?
Advancing practice is a level of practice in which a practitioner has demonstrated their ability to work autonomously at a high level (level 7/master’s level) across all four pillars of advancing practice.
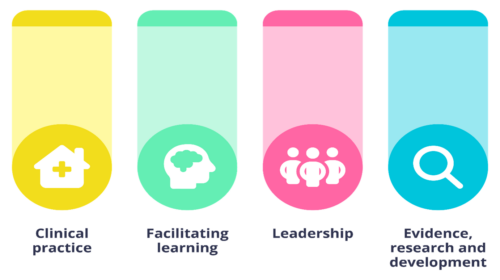
The four pillars
The four pillars of advancing practice are clinical practice, leadership and management, education, and research.
Advanced clinical practitioners (ACPs) can be found across a range of professional backgrounds and settings. The term ACP is a consensus umbrella term to encompass the wide range of registrants who work in advancing practice roles, often with variable job role titles. Advancing practice may also vary between the devolved nations.
Terminology
The two most commonly used acronyms in advancing practice are ACP and AP. These stand for:
- ACP or advancing clinical practice/advanced clinical practitioners = role
- AP or advancing practice = a level of practice
There also can be some confusion between the difference of an ACP and consultant.
ACP
An ACP would be expected to be a leader, educator, highly skilled clinician, and to have an understanding of the wider health and care system and how that impacts on their practice.
Within the education pillar, it is the expectation that the ACP is an educator and that the capabilities are focused on the team and the educational role of the ACP, with some reference to contributing to a culture of learning.
ACPs are expected to critically engage in research activity, adhering to good research practice guidelines, so evidence-based strategies are developed and applied to enhance quality, safety and productivity and value for money.
Consultant
A consultant on the other hand, is a leader, enabler and facilitator of education and learning, clinical excellence, research/improvement and leadership across the system.
For a consultant, the focus is more about leading and enabling a system-wide culture of learning.
The purpose of the pillar is defined as ‘developing staff potential’, adding to and transforming the workforce, and helping people to learn, develop and improve (in and from practice) to promote excellence’, and this is further illustrated by ‘actively creating a learning culture across the system’.
RCSLT position statement
The RCSLT produced a position statement on advancing practice and consultant practice in September 2019. It states that:
“The RCSLT Board of Trustees considers that these roles will offer important new opportunities for career progression to speech and language therapists (SLTs). They will also make an important contribution to improving service quality and accessibility for service users to timely treatment.”
The RCSLT promotes:
- ACP and consultant practice as a level of practice, rather than as particular roles.
- Ways to ensure that SLTs already in these roles (whether or not their title reflects that) are able to access credentialing opportunities – in England it is being proposed that it will be possible to demonstrate practice at the required level by means of an accredited portfolio.
- That not being able to prescribe should not preclude SLTs from taking on ACP roles. In some cases patient group direction can provide a solution.
- That ACP frameworks cannot contain prescribing as a mandatory requirement if they are to be multi-professional. It must be optional or it will exclude some AHPs.
- Greater clarity about where ACP roles fit within career pathways and how they are different from specialist roles. In our view there remains some ambiguity over the distinction between advanced clinical practice and clinical specialism.
- The development of processes and systems that work UK-wide for recognising individual practitioners’ fulfilment of advanced-level capabilities. – Or alternatively, the development of parallel approaches that reduce the risk of misaligned approaches and achieve clarity for all stakeholders.
- Better capture of data on SLTs working in these roles.
- Recognition that SLTs can take on ACP roles across a range of settings, from acute to community, and across adult and children’s services, and that these roles are not limited to taking on roles of other medical staff.
The RCSLT:
- Aims to provide clarity for SLTs on post-registration career development opportunities developing in advancing practice, consultant roles, clinical academics and specialisms.
- Would like SLTs to be aware of, and take advantage of, the progression and career opportunities offered by recent developments being driven by NHS England (formally HEE) and other organisations.
- Would like to set those developments in the context of the SLT role and consider next steps to support the profession.
Benefits of the role to profession
There are many benefits of becoming an ACP and having an ACP in the team:
- The role demonstrates clear career progression.
- It enables staff to receive acknowledgement for work that they are already doing that demonstrates advancing practice competencies. Having healthcare professionals at advancing levels increases capacity and capability within services.
- By integrating into multi-professional teams, ACPs provide clinical leadership and enable collaboration across the multi-disciplinary team through complex decision making and managing risk. This also gives organisations a flexible workforce to meet changing population, patient, and service delivery needs.
- ACPs help to improve clinical continuity and provide high-quality care for patients.
- They enable workforce transformation to initiate a wider range of advancing clinical care being provided by a varied range of multi-professional clinicians rather than focusing on medical doctors as the sole providers of advancing clinical care.
- ACPs can accelerate access to care for patients and help to improve outcomes.
Advancing practice and service development
Developing an ACP role needs careful consideration. Thought needs to be given as to whether an ACP role can meet the needs of a service.
There may only be a demand for one AHP ACP within a multidisciplinary team. A clear rationale for this role needs to be set out. Services may wish to identify a role for an ACP trainee to progress to ensure the CPD of the trainee, as well as to meet the anticipated needs of the service. SLTs are able to offer a breadth of skills in this space.
It is important to remember that in terms of career progression, SLTs are not missing out on opportunities if they do not become ACPs. Highly specialist roles are always important.
Two SLTs could be working at the same band or level with:
- one in an ACP role
- one in a highly specialist role
Progression to consultant level is possible via both roles.
SLTs are encouraged to also review the professional development framework, which contains tools that allow mapping of your existing skills and experience against the four pillars of practice: professional practice, leadership and management, evidence, research and innovation, and facilitation of learning.
Enhanced practice
Enhanced practice is an enhanced level of practice which is delivered by established, autonomous practitioners covering clinical duties, leadership, education and research. They would be expected to use their profession specific knowledge and skills to make autonomous decisions within a defined clinical space whilst managing and mitigating risk to the patient, colleagues and service.
Enhanced Practice may be the target destination for some clinicians but it also acts as good preparation for those who may want to become an AP or consultant.
