Autism overview
(Last updated October 2023)
This public page aims to provide clarity on the role of the SLT working with autistic people and support networks for families, other professional groups, commissioners, and policy makers.
About
This guidance was co-produced by autistic people, parents of autistic children and adults, and speech and language therapists (SLTs). Two versions were produced, the first aimed at providing guidance specifically for SLTs and this version for the wider public. We have acknowledged the range of presentations and co-occurring diagnoses in our recommendations. This means, for example, that some recommendations relate to all autistic people and others are relevant specifically for autistic people with a learning disability.
In addition to these pages which have been written to provide clarity on the role of SLTs working with autistic people, we have also provided clinical-level guidance for our members.
The member guidance aims to support SLTs to:
- recognise, assess, and offer intervention and support to autistic people.
- to place the lived experiences of all autistic people and their families at the centre of practice, to advocate for reasonable adjustments and to recognise, avoid, counter and challenge discrimination.
SLTs have been encouraged to approach this guidance with an awareness that knowledge and understanding of autism and autistic people continues to evolve within the fast-changing field of neurodiversity, and with a diversity of views. Using evidence-based practice, SLTs are encouraged to think sensitively and reflectively, base clinical decisions around the needs and preferences of each individual child or adult and approach all sources of information with an open and critical mind, being aware that there may be newer information and perspectives to consider.
This public page aims to:
- provide clarity on the role of the SLT working with autistic people and support networks for families, other professional groups, commissioners, and policy makers.
What is autism?
Autism is a disability affecting neurodevelopment and characterised by differences in social interaction, in speech, language and communication; in learning, thinking and processing; in experiencing feelings; in intensity of interests and sensory processing. Some but not all autistic people identify as disabled. Autism can be present in families across generations, passed on through genetics and continues throughout a person’s life. There is a wide variation in autistic characteristics and how these impact a person’s day to day experiences and life in general. An individual’s strengths and needs change throughout their life and depend on many factors including the environment. These individual variations can be thought of as a wheel (see Figure 1).
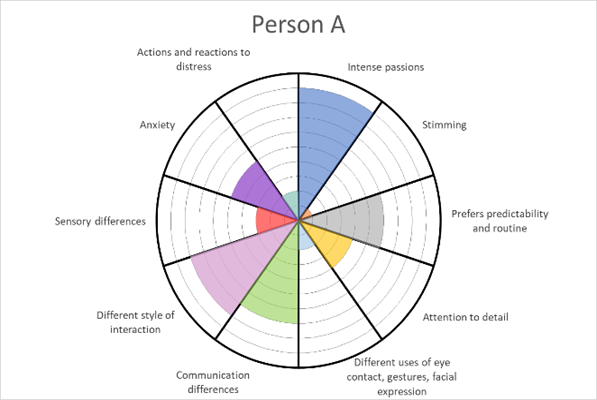
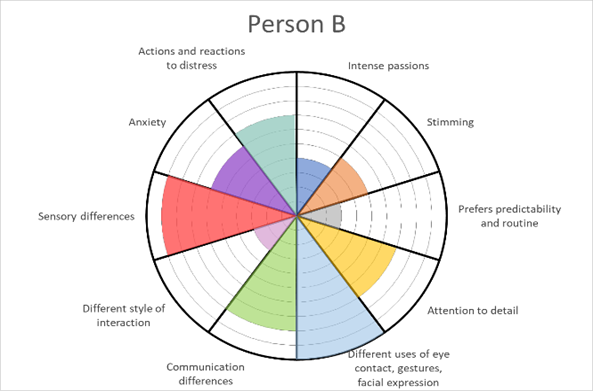
Figure 1: Wheel depiction of the autism spectrum, showing the different profiles of two hypothetical autistic people (created for this guidance by Williams and Baxter).
Autism is usually associated with typical intelligence where it is considered part of the range of natural variation in brain development, bringing both strengths, and challenges that may require support.
Across the world, there are varying estimates of the rates of diagnosis, but they are increasing. For example, worldwide estimates range from 0.6 – 1 in 100 being autistic (Salari et al 2022; Zeidan et al 2022), and in Scotland, using the 2011 Census, 1.6% of the population indicated that they were autistic (Kinnear et al 2020).
The reported global proportion of autistic individuals assigned males at birth to individuals assigned females at birth is estimated to be 2 males to 1 females (“4:2” Zeidan et al 2022).
Rates of autism diagnosis are increasing in the UK, particularly in adults in general, in individuals assigned females at birth, and those without learning disability (Russell et al 2022; in Wales: Underwood et al 2022), with some dramatic changes over time noted (Hughes et al 2023). The rates of those with learning disability and the highest support needs continue to rise but more slowly (Hughes et al 2023). This suggests that the overall rise in the number of autistic people identified may be associated with changes in diagnostics.
It is common for an autistic person to have more than one neurodevelopmental diagnosis, as well as others such as those affecting mood, and physical health needs such as epilepsy. Common co-occurring diagnoses include learning disability, Language Disorder, Attention Deficit Hyperactivity Disorder (ADHD) and Developmental Coordination Disorder (DCD) (see NICE guidance CG128, CG142 in the resources page).
Globally, the proportion of those diagnosed with a co-occurring learning disability is estimated at 33% (Zeidan et al 2022). In Scotland, 20% of autistic people were estimated to have an additional learning disability (Kinnear et al 2020).
Many people are disabled by their autism and/or by other co-occurring diagnoses, with as many as 50% of individuals with high support needs (Lord et al 2022) that continue throughout life. For children with a learning disability in the US, the proportion of those with the highest support needs was estimated to be 28%. These children require around the clock supervision, are non-speaking and often with epilepsy and self-injury (Hughes et al; 2023).
NOTE: The aforementioned statistics are only estimates at a single point in time and have acknowledged limitations due to for example, research methodologies, variability in estimates, evolving trends in who are receiving diagnoses, the likelihood of under diagnosis in certain ethnic groups (e.g. de Leeuw, Happé & Hoekstra 2020) and lack of acknowledgement of gender diversity.
As with all people, autistic people have their own individuality, personality and strengths which can change and develop across the life-course influenced by their experiences through life, society and the wider environment. In recognition of these influences:
- Autism features can differ across ages, for example hand mannerisms that might have been predominant in a young autistic child might be less so in an adult, possibly due to an autistic person intentionally or unintentionally camouflaging or masking this feature.
- The cultural context is important. The broad areas of difference in autism are thought to be the same across different ethnic groups around the world but the specific features or examples, and impact on daily living, can differ (Carruthers et al 2018).
- Autism presentations can differ. An alternative presentation of autism was identified in response to the under recognition of individuals assigned female at birth (AFAB). This is now known not to be gender exclusive as individuals assigned male at birth (AMAB) may also present this way (Pearson and Rose, 2021). This may (or may not) be in the absence of gender identity differences. This presentation is sometimes described as ‘masked’ autism (for an explanation about masking see Pearson & Rose 2021, and our resources section). These individuals may (Hull, L., Petrides, K.V. and Mandy, W., 2020):
- have a greater interest in forming relationships but struggle to maintain them.
- have fewer repetitive behaviours or intense passions, or that these passions might be harder to notice because they may appear more culturally acceptable.
- internalise emotional difficulties potentially giving rise to anxiety, depression in contrast to externalising them through, for example, aggression.
- use conscious or unconscious strategies to hide any differences when in social situations. This camouflaging and masking can also affect a person’s mental wellbeing and can be driven by anxiety in response to the attitudes and responses of others (Chapman et al 2022).
Over time, a number of psychological theories of autism have been proposed such as theory of mind, executive functioning, central coherence, sensory processing accounts, each with strengths and limitations. It is beyond the scope of this guidance to discuss all of them, however, we highlight the double empathy problem (Milton 2012) and monotropism (Murray, Lesser & Lawson; 2005), considered by many autistic people as central to understanding autism, supporting autistic individuals and assisting non-autistic people in their interactions with autistic people.
The Double Empathy problem assists in understanding the effect of non-autistic communication styles when interacting with an autistic person. Monotropism refers to the tendency to be pulled into one’s interests more intensely thus leaving fewer processing resources for other things. This allows people to respect the value of such passions for example in educational advancement and participation. It can help people recognise that moving from a task involving a particular interest to another might be hard for an autistic person and that integrating a person’s interests into tasks may be beneficial (Wood 2021; Ninci et al 2020).
Promoting equity for autistic people: neurodiversity statement
We live in a society enriched by diversity, including neurodiversity. Neurodiversity refers to the many ways that people can experience and interact with the world due to differences in their brains; together we are all neurodiverse. Speech and language therapists (SLTs) recognise this and value the rights of all people to make their own decisions and follow their own interests. Some individuals’ brains diverge from what is typical, resulting in a diagnosis for some. Autism is one of these ‘neurodivergences’ or ‘neurotypes’ and as such is a ‘neurominority’.
Our society is largely better suited for the neuromajority and SLTs therefore commit to taking deliberate steps to develop neurodiversity affirming practice within our profession. Understanding the needs and preferences of neurominorities such as autistic people will be at the centre of speech and language therapy provision. SLTs will recognise an autistic person’s support needs and disability, understanding that to thrive, a person’s environment must meet their individual needs. This commitment includes understanding the ways in which autistic people are excluded or included in society, how adjustments can be made to everyday expectations, interactions and environments, and how specific skills can be taught where this improves a person’s quality of life and reduces any risks to them. In particular, our profession has a key role in making communication experiences as meaningful as they can be.
NOTE:
- For a brief introduction to neurodiversity, the neurodiversity paradigm, the neurodiversity movement and terminology please see the member guidance
- For a definition of terminology please see the Glossary
How can speech and language therapy help?
A range of professionals and services will be variably involved with an autistic person over the course of their life. Working in partnership with others across all levels is central to improving outcomes for autistic people. This includes collaboration with other professionals and co-production with those with lived experience of autism, including parents/carers of autistic children where relevant in developing services and conducting research. Involvement of autistic people has been historically lacking in these areas but with emerging progress and calls for change (e.g. Pukki et al 2022). Partnership working with an autistic person and others includes understanding and respecting different perspectives, aiming for shared views and goals. The RCSLT has guidance for SLTs on collaborative practice.
SLTs, some who may be autistic themselves, have expertise across the lifespan in language (speaking, understanding, processing), communication, interaction and eating and drinking. This includes an understanding of how these capabilities develop, the contribution of the environment (which includes people) and any changes as people age. SLTs can contribute towards understanding and managing distress and mental wellbeing, empowering the individual and supporting self-advocacy, assist in developing safe and consenting and meaningful relationships, helping autistic people understand their own autistic experience, addressing the impact of a person’s differences across environments, empowering others in the support of the individual, leadership and advocacy across and within systems such as health, education, social care, the Voluntary, Community and Social Enterprise (VCSE) sector and in research.
SLTs work with individuals, their parents/carers, other professionals and support staff in a variety of settings and systems such as homes/care homes, educational settings across the ages including home schooling and education other than at school (EOTAS), apprenticeships/work, accommodation, secure facilities, forensic services, the criminal justice system, and mental health facilities so that autistic people can:
- have their communication, language, eating and drinking needs identified early
- express themselves, be understood and understand others to participate in their everyday life
- have their needs and preferences understood by those around them who are in turn equipped to meet them by adapting their own style of communication
- understand themselves, to self-advocate and when necessary, learn essential communication skills to support their autonomy
- feel able to develop meaningful relationships.
This supports autistic people to:
- learn, work and play
- feel valued, accepted and included
- feel healthy, secure and safe
- have autonomy and agency and achieve as much independence as they can and want.
What can you expect from speech and language therapy?
How speech and language therapy is provided
We recognise that speech and language therapy is currently a shortage profession. We are also aware that in 2023 vacancy rates are high, averaging at 23% across the nations. These two factors significantly affect the availability of this type of support to all people with speech, language and communication needs and including autistic individuals. The RCSLT continues to advocate with governments and agencies for adequate resources and support wherever needed.
Services are organised in a variety of different ways. The number of speech and language therapists (SLTs) in a service is also variable but the numbers employed by the NHS typically decrease from early childhood to adulthood, with a similar reduction in the availability of SLTs who consider themselves specialists in autism. SLTs can usually access routine clinical supervision, peer support, local specialists and/or RCSLT national clinical advisors, and RCSLT Clinical Excellence Networks, should a person’s specific needs not be within their experience or expertise.
SLTs can be employed by the NHS, education authorities, individual schools or are independent practitioners either solely or as a part of a company. Some may work in multiple settings with different roles including in Higher Education Institutions and in research. These variations can affect their availability, roles and responsibilities based on differences in what they are commissioned or paid to do.
SLTs may work directly with an individual and/or their parent/carer, or indirectly advising and supporting key people in the autistic person’s life.
Children and young people
- Many NHS speech and language therapy services welcome referrals, or requests for assistance, directly from parents or carers; GPs and other health or education professionals can also refer. Individual services may have specific criteria or procedures for such referrals.
- Specialist care and education organisations may have different funding models for SLT provision whereby SLT is included within an established placement funding model.
- Children’s NHS speech and language therapy services are often organised around three levels: universal (available to all children), targeted (to a group who have been identified as at risk of a communication problem) and specialist (for children with identified needs) but definitions of service delivery within these areas are locally defined. A child may access support from all levels.
- SLTs employed by education authorities or schools may only be employed to provide support to autistic children within the school setting; this would include liaison with parents/carers.
Adults
- In adult services currently, there are specialist speech and language therapy services that sit within learning disability services, diagnostic services, services in criminal justice liaison and diversion, mental health services and inpatient/acute services.
- In some of those services, speech and language therapy may not be commissioned for therapeutic support despite clear needs.
- GPs or social workers can make a referral to adult speech and language therapy if it is commissioned in their local area. Within specialist settings, they may also be referred by other healthcare professionals. In England, where the young adult has an Education Health Care Plan (EHCP), speech and language therapy may be accessed in the education setting. An individual may also choose to self-fund and utilise the services of independent SLTs(see The Association of Speech and Language Therapists in Independent Practice (ASLTIP)).
- When a person receives a diagnosis of autism and learning disability in childhood, they can access adult learning disability services at age 18, which can include speech and language therapy.
- If an autistic person does not have a learning disability, services (including speech and language therapy) may only be available if they have mental health needs, if they stammer or are non-speaking and use AAC.
- Autistic adults who stammer can access speech and language therapy, although NHS provision and waiting times vary across the country. For other options see options for Adults (18+) (STAMMA) and RCSLT information on Dysfluency.
- In some adult services in England, young people with education, health and care plans (EHCPs) are referred to speech and language therapy. However, differences in the roles that SLTs are commissioned to perform can mean they are not able to deliver the specified EHCP outcomes. This does not mean the EHCP outcomes are incorrect, and it will be the responsibility of the local education authority to provide and/or find a therapist, up to the age of 25 years. Should a parent/carer in England require support in accessing speech and language therapy in this situation (and for children), the following organisations may help: SOS!SEN – The Independent Helpline for Special Education Needs and IPSEA – Independent Provider of Special Education Advice.
For children and adults, families or individuals who wish to directly arrange speech and language therapy support can do so via ASLTIP, the Association of Speech and Language Therapist in Independent Practice.
Assessment and diagnosis
All autistic people have different styles of language and communication, but any differences may only affect participation in life for some people. For those, assessment by an SLT is an essential component of identifying the specific support needs of that person. Communication differences can contribute to a person’s mental wellbeing, their education and life chances. SLTs also form a vital part of a diagnostic team, with NICE and NHSE guidance recommending suitably trained professionals to be able to differentially diagnose and identify co-occurring diagnoses relating to speech, language and communication (see NICE guidance CG128, CG142). Assessment will:
- be person-centred, with the specific aims well defined and agreed with the autistic person and/or their representative if they are unable to do so utilising the process of establishing a ‘best Interest’ decision. (See NICE Guidance on Decision-making and mental capacity and RCSLT Guidance on Supported decision making and mental capacity).
- be open to the wide variety of presentations in autistic people.
- be holistic, combining information from a variety of sources including, when possible, seeking the views and perceptions of the person being assessed. Identifying which of the many available methods of assessment available to an SLT, will be based on presenting needs of the person and context.
- include an understanding of an individual’s support network and environment and how these might contribute to, or support, a person’s current needs.
- identify opportunities for change to improve or enhance outcomes for the individual, identifying reasonable adjustments.
- consider the ways in which a person’s language, communication, social cognitive needs and the impact of the environment contribute to that person’s regulation of their emotions and understanding of distressed behaviours when they are present.
- contribute to a multi-disciplinary diagnostic assessment.
In a diagnostic assessment, an SLT can:
- contribute to diagnostic formulation and understanding of the person as a whole e.g. the impact of communication on risk, mental health and recommendations for reasonable adjustments to meet needs.
- assess and identify language, social communication and interaction differences and their impact.
- recognise speech sound difficulties and their impact.
- recognise the impact of a stammer, if present.
- contribute to assessment and observation of learning abilities, sensory preferences, mental health, how a person acts and responds in different situations and how a person’s speech, language and communication needs may contribute.
- differentially diagnose Developmental Language Disorder (DLD) (see RCSLT DLD guidance).*
- identify Language Disorder as a co-occurring diagnosis (see Co-occurring DLD or Language Disorder Associated with…?)*
- share with the assessment team the potential contribution these differences may have on other aspects of assessment and on the difficulties the individual is experiencing.
*NOTE: Some diagnostic services are diagnosis specific affecting the capacity of an SLT to carry out additional assessment to confirm these diagnoses. In this situation SLTs will be able to identify concerns and risks and refer to the broader SLT service. In some situations, assessments may have been completed by colleagues prior to the diagnostic assessment, providing evidence to support diagnostic decision making.
Intervention and support
Please note: any interventions mentioned on this page are provided for informational purposes only. No endorsement is expressed or implied.
Principles of neurodiversity-informed intervention and support
- SLTs have a responsibility to openly discuss options for support and intervention with autistic people and/or their parents or carers where appropriate. These balanced discussions should include advantages, disadvantages and current thinking on particular approaches to ensure that choice is well informed and meets the needs of the specific individual.
- Interventions and outcomes are an agreed preference and priority of the autistic individual and/or their parent/carer/advocate where they are unable to make this decision. In adults without the capacity to consent, decisions about interventions and outcomes will be in their best interest (see NOTE below).
- Successful communication and interaction depends on all people involved, including the autistic person and everyone in their environment. SLTs have a role supporting communication and interaction changes and adaptations in all relevant people.
Neurodiversity-informed interventions:
- focus on harnessing a person’s strengths, interests and abilities and functional needs.
- aim to improve a person’s quality of life and reduce risk.
- aim to provide support and adaptations that affirm an individual’s neurodivergent identity.
- are personalised to the needs of that autistic person at that time; no single approach is recommended for all autistic people all the time.
- are evidence-informed (triangulating best scientific evidence, clinical experience and the individual’s values).
- are trauma-informed, taking account of any Adverse Childhood Events (ACEs) and any other trauma inducing experiences, and personalised to avoid risk of re-traumatisation.
NOTE:
Best interest decisions are made when an adult is judged not to have capacity for a specific decision (See NICE Guidance on Decision-making and mental capacity and RCSLT Guidance on Supported decision making and mental capacity). People over the age of 16 who do not have capacity (see Mental Capacity Act 2005) are supported to be as involved as possible in decision making (see RCSLT Learning Disabilities Guidance). SLTs have a role in supporting reasonable adjustments for any language and communication factors that may be a barrier to decision making for a person over the age of 16.
For consent to treatment in children please see: Consent to treatment – Children and young people (NHS).
Areas of intervention and support
1. Language
SLTs can:
- support opportunities to facilitate the development of all aspects of structural language, particularly in children and young people.
- ensure that the choice of language goals is meaningful to the autistic person e.g. vocabulary related to their current interests.
- advocate for the use of Alternative Augmentative Communication for non-speaking individuals and those with few words with or without a learning disability (see RCSLT AAC guidance) where needed e.g. objects of reference, manual signs, paper-based and electronic systems including Apps.
2. Social communication and understanding
SLTs can:
- support an autistic person to have a meaningful way of communicating their needs across different environments and at different ages such as sharing their interests, developing friendships and being able to self-advocate.
- support self-advocacy and for people with few or no (spoken) words by co-developing and using personal passports (see e.g. Personal Communication Passports, My Healthcare Passport (NHS East Kent Hospitals University Foundation Trust) and Talking Mats).
- support an autistic person in managing and navigating particular social situations including self-advocacy, if they ask for assistance in this specific situation.
- support an autistic person in social understanding work if this is something they want to engage in – both in anticipation of planned social interactions and reflecting on past social experiences, encouraging self-advocacy and their and others’ understanding of the double empathy problem.
- offer culturally sensitive training or coaching to people about autistic communication styles including supporting non-autistic people to recognise their own bias in interacting with autistic people (Sasson et al 2017). This could include facilitating a self-prompt approach (see Silver & Parsons 2015 and 2022) or adult interaction approaches or parent-child interaction approaches. Examples used across the UK include intensive interaction (Hutchinson & Bodicoat 2015), Paediatric Autism Communication Therapy (PACT) (Green et al 2010; Pickles et al 2016) and More Than Words® (More Than Words – Hanen Program for Parents of Children on the Autism Spectrum). When working directly with parents using parent-child interaction approaches, SLTs will consider the family’s current capacity to take on extra demands related to such interventions and offer alternatives if appropriate.
3. Actions and responses suggestive of distress and emotional regulation
‘Actions and responses suggestive of distress’ have been previously referred to, for example, as ‘behaviour that challenges’ or ‘challenging behaviour’; we recognise that in wider society these terms may still be in use.
SLTs have a role in identifying and adapting communicative and environmental factors, including recognising sensory components, that may contribute to an autistic person reacting with distress, for example by hurting themselves or others, running away, damaging property and ruminating on their understanding of social relationships and interactions. This includes understanding how this distress may relate to unmet needs, an autistic person’s preferences and what the person is trying to communicate through their actions. It will include identifying environmental factors and suggestions for modifying the contributors to that distress.
These types of actions and responses can be viewed in a negative way by those they affect, particularly if they are directed towards, or cause harm to another person. This can often result in a breakdown in the relationship between the autistic person and those around them, risking the loss of friendships or supportive relationships. Public perception of such actions and responses can also be negative. If the person’s differences and support needs are not understood by the person who is observing the actions then there is a possibility that these will be viewed as criminal acts, particularly when they have caused damage to public property or harm to another person.
SLTs can:
- contribute to achieving a shared understanding of why a person is expressing distress by identifying all possible contributory factors.
- support the person’s ability to communicate their needs safely and self-advocate. This may include teaching an alternative way to express a particular need or make a request.
- ensure that the social and physical environment meets the needs of the autistic person through making reasonable adjustments (see below).
- support all involved parties in including the autistic person’s point of view, and if the autistic person has identified that they are ready to, to understand the differing perspectives on the situation to support relationship repair.
- provide support to prevent communication breakdown during contact (of any kind) with the justice system. Where possible SLTs may support the autistic person’s understanding of the criminal justice system and relevant sections in the mental health act.
- support the criminal justice system to understand the contribution of communication differences when actions or responses suggestive of distress or social communication breakdown is viewed or interpreted as criminal. This includes advising on reasonable adjustments and how this relates to vulnerabilities. See RCSLT Justice guidance.
For further information see our resources section.
4. Environmental supports and reasonable adjustments
SLTs can contribute to identifying necessary environmental adaptations and reasonable adjustments, advocating for a neurodiversity affirming environment. This includes the use of visual supports (objects, photos, pictures, the written word), managing the sensory environment, making the environment predictable and reliable and ensuring others understand the communication needs of the autistic person including making adjustments to their own use of language and interaction style.
For further information see our resources section.
5. Teaching strategies
Neuro-affirmative interventions aim to improve subjective quality of life and support the developmental trajectory of an autistic person even if that trajectory is affected by co-occurring diagnoses. To achieve this, there will be situations where specific skills or strategies will need to be taught and/or where an autistic person may actively request to learn a strategy even when it is not an area of strength. For example, teaching skills that support an autistic person to meet their own basic needs and self-advocate such as communicating what they want, to say no, to be able to leave, to ask for the toilet or specific social skills such as interview skills or attending doctor’s appointments. Some autistic people hold the view that neurotypical communication shouldn’t be taught but others also say that knowing social norms is empowering.
SLTs can support the teaching of specific language and communication skills and strategies:
- when an autistic person asks them to
- when the parent/carer of an autistic child asks, ensuring the child and young person is involved in the decision making
- when it is in the autistic person’s best interest following a ‘Mental Capacity Assessment’, enhances quality of life and/or reduces risk.
NOTE: Critical discussion related to some interventions
In its guidance for members, the RCSLT have included references to some interventions that are not supported by some advocates of the neurodiversity movement. This is to ensure that SLTs are informed both to support their own critical thinking in evidence-based practice, and in supporting shared decision making with autistic people and their parents or carers, including when a ‘best interest’ decision is being made.
The interventions relate to behaviour-based interventions and social skills training. From a neurodiversity perspective these approaches are considered to promote the teaching of neurotypical ways of being i.e. normalisation, which is considered discriminatory against a neuro-minority way of being and, for some interventions, there is emerging evidence of harm.
We acknowledge that not all autistic people agree and some autistic people and/or their parents choose these interventions.
6. Supporting transitions
SLTs can have a key role in supporting successful transitions for autistic people, who may experience difficulties when doing so. Transitions can be defined broadly to include any movement or change of place, for example between home and education setting, between classrooms, or rooms in supported living accommodation; between different education settings e.g. from primary to secondary school and transition to adult services, getting a new job or moving house.
SLTs can:
- support the development of a co-produced transition document for an autistic person
- ensure information about an autistic person’s needs including their communication profile including any use of augmentative and alternative communication (AAC), visual supports, and any identified reasonable adjustments are documented, shared and support their implementation.
See: Transition to adult services and autism (SCIE); for advice across the UK nations and tips see Transitions (National Autistic Society).
Resources and glossary
See glossary of terms and resources in our member guidance. Please note, many of these resources are aimed at SLTs, and the glossary is based on terms used in the guidance for SLTs – some of which may not be used in this public page.
Contributors
Lead Author
Dr Penny Williams – Consultant Speech and Language Therapist
Supporting Authors
Paul Burdon – Highly Specialist Speech and Language Therapist
Scarlet Clark – Autistic adult
Tamsin Green – Parent of autistic young person
Lesley Jenkins – Parent of young autistic person
Heidi Keeling – Speech and Language Therapist
Dr Sarah Markham – Visiting Researcher, Institute of Psychiatry, Psychology & Neuroscience (IoPPN), King’s College London
Katie Pears – Speech and Language Therapist
Gaia R (she/her) – Autistic adult, neurodiversity advocate and mental health clinician
Vicky Romilly – Speech and Language Therapist
Dr Marion Rutherford – Speech and Language Therapist and Senior Research Fellow, National Autism Implementation Team Lead (Scotland)
Naomi S – Speech and Language Therapist, autistic adult and parent of autistic children
Aysha Siddika – Speech and Language Therapist
Kerry Stewart – Parent to neurodivergent children, neurodivergent adult, neurodivergent Psychologist
References
- Carruthers, S., Kinnaird, E., Rudra, A., Smith, P., Allison, C., Auyeung, B., Chakrabarti, B., Wakabayashi, A., Baron-Cohen, S., Bakolis, I. and Hoekstra, R.A., 2018. A cross-cultural study of autistic traits across India, Japan and the UK. Molecular autism, 9, pp.1-10.
- Chapman, L., Rose, K., Hull, L. and Mandy, W., 2022. “I want to fit in… but I don’t want to change myself fundamentally”: A qualitative exploration of the relationship between masking and mental health for autistic teenagers. Research in Autism Spectrum Disorders, 99, p.102069.
- Green, J., Charman, T., McConachie, H., Aldred, C., Slonims, V., Howlin, P., Le Couteur, A., Leadbitter, K., Hudry, K., Byford, S. and Barrett, B., 2010. Parent-mediated communication-focused treatment in children with autism (PACT): a randomised controlled trial. The lancet, 375(9732), pp.2152-2160.
- Hughes, M.M., Shaw, K.A., DiRienzo, M., Durkin, M.S., Esler, A., Hall-Lande, J., Wiggins, L., Zahorodny, W., Singer, A. and Maenner, M.J., 2023. The Prevalence and Characteristics of Children With Profound Autism, 15 Sites, United States, 2000-2016. Public Health Reports, p.00333549231163551.
- Hull, L., Petrides, K.V. and Mandy, W., 2020. The female autism phenotype and camouflaging: A narrative review. Review Journal of Autism and Developmental Disorders, 7(4), pp.306-317.
- Hutchinson, N. and Bodicoat, A., 2015. The effectiveness of intensive interaction, a systematic literature review. Journal of Applied Research in Intellectual Disabilities, 28(6), pp.437-454.
- Kinnear, D., Rydzewska, E., Dunn, K., Hughes-McCormack, L.A., Melville, C., Henderson, A. and Cooper, S.A., 2019. Relative influence of intellectual disabilities and autism on mental and general health in Scotland: a cross-sectional study of a whole country of 5.3 million children and adults. BMJ open, 9(8), p.e029040.
- Lord, C., Charman, T., Havdahl, A., Carbone, P., Anagnostou, E., Boyd, B., Carr, T., De Vries, P.J., Dissanayake, C., Divan, G. and Freitag, C.M., 2022. The Lancet Commission on the future of care and clinical research in autism. The Lancet, 399(10321), pp.271-334.
- Milton, D.E., 2012. On the ontological status of autism: the ‘double empathy problem’. Disability & Society, 27(6), pp.883-887.
- Murray, D., Lesser, M. and Lawson, W., 2005. Attention, monotropism and the diagnostic criteria for autism. Autism, 9(2), pp.139-156.
- Ninci, J., Neely, L.C., Burke, M.D., Rispoli, M., Vannest, K.J., Willson, V. and Ulloa, P., 2020. A meta-analysis of single-case research on embedding interests of individuals with autism spectrum disorder. Remedial and Special Education, 41(5), pp.296-308.Pearson, A. and Rose, K., 2021. A conceptual analysis of autistic masking: Understanding the narrative of stigma and the illusion of choice. Autism in Adulthood, 3(1), pp.52-60.
- Pickles, A., Le Couteur, A., Leadbitter, K., Salomone, E., Cole-Fletcher, R., Tobin, H., Gammer, I., Lowry, J., Vamvakas, G., Byford, S. and Aldred, C., 2016. Parent-mediated social communication therapy for young children with autism (PACT): long-term follow-up of a randomised controlled trial. The Lancet, 388(10059), pp.2501-2509.
- Pukki, H., Bettin, J., Outlaw, A.G., Hennessy, J., Brook, K., Dekker, M., Doherty, M., Shaw, S.C., Bervoets, J., Rudolph, S. and Corneloup, T., 2022. Autistic perspectives on the future of clinical autism research. Autism in Adulthood, 4(2), pp.93-101. Zeidan, J., Fombonne, E., Scorah, J., Ibrahim, A., Durkin, M.S., Saxena, S., Yusuf, A., Shih, A. and Elsabbagh, M., 2022. Global prevalence of autism: a systematic review update. Autism Research, 15(5), pp.778-790.
- Russell, G., Stapley, S., Newlove‐Delgado, T., Salmon, A., White, R., Warren, F., Pearson, A. and Ford, T., 2022. Time trends in autism diagnosis over 20 years: a UK population‐based cohort study. Journal of Child Psychology and Psychiatry, 63(6), pp.674-682.
- Salari, N., Rasoulpoor, S., Rasoulpoor, S., Shohaimi, S., Jafarpour, S., Abdoli, N., Khaledi-Paveh, B. and Mohammadi, M., 2022. The global prevalence of autism spectrum disorder: a comprehensive systematic review and meta-analysis. Italian Journal of Pediatrics, 48(1), pp.1-16.
- Sasson, N.J., Faso, D.J., Nugent, J., Lovell, S., Kennedy, D.P. and Grossman, R.B., 2017. Neurotypical peers are less willing to interact with those with autism based on thin slice judgments. Scientific reports, 7(1), pp.1-10.
- Silver, K. and Parsons, S., 2015. Noticing the unusual: A self-prompt strategy for adults with autism. Advances in Autism.
- Silver, K., & Parsons, S. 2022. Perspectives of autistic adults on the strategies that help or hinder successful conversations. Autism & Developmental Language Impairments, 7. https://doi.org/10.1177/23969415221101113.
- Underwood, J.F., DelPozo-Banos, M., Frizzati, A., John, A. and Hall, J., 2022. Evidence of increasing recorded diagnosis of autism spectrum disorders in Wales, UK: An e-cohort study. Autism, 26(6), pp.1499-1508
- Wood, R., 2021. Autism, intense interests and support in school: From wasted efforts to shared understandings. Educational Review, 73(1), pp.34-54.
- Zeidan, J., Fombonne, E., Scorah, J., Ibrahim, A., Durkin, M.S., Saxena, S., Yusuf, A., Shih, A. and Elsabbagh, M., 2022. Global prevalence of autism: A systematic review update. Autism Research, 15(5), pp.778-790.
 Download as PDF
Download as PDF
