This information aims to promote understanding and raise awareness about the context of working life for people with a disability, difficulty or difference.
About this guidance
This information has been prepared with the help of the RCSLT Disability Working Group. A huge thank you to them for sharing their time, resources and expertise to put this together.
We hope it is useful for all speech and language therapists (SLTs), speech and language therapy assistants (SLTAs) and students, whether or not you have a disability, and that it will help promote understanding and raise awareness about the context of working life for people with a disability, difficulty or difference.
It is intended to provide practical information and tips on supporting SLTs with a disability in the workplace. We hope this will help both SLTs and their managers to discuss, develop and implement workable, practical adjustments to enable all SLTs with a disability to participate fully in their workplace.
This document does not provide legal advice, but links to relevant pieces of legislation are included for completeness.
“You can treat disabled people better or ‘more favourably’ than non-disabled people and sometimes this may be part of the solution.”
– The Equality and Human Rights Commission
Large print version
- Guidance – large print version (PDF)
- Case studies – large print version (PDF)
- Resources – large print version (PDF)
Who is this guidance for?
This document will be of particular interest to SLTs and SLTAs with a disability and their managers, admissions tutors to speech and language therapy training courses, HR departments and Occupational Health departments. It will also be relevant to student SLTs with a disability and placement educators in the context of placements.
Where this document refers to SLTs it also refers to SLTAs, unless the context relates to qualified SLTs only.
We hope that colleagues of SLTs with a disability will also find this useful in terms of raising awareness of the issues and being able to speak up if they see discrimination.
Context of this guidance
The Department for Work and Pensions Family Resources Survey 2018-19 reported that 19% of working age adults have a disability. Around 39% of this group in turn reported mental health impairments.
While we do not know at present how many SLTs have a disability, we do know from student SLT data that, in 2018-19, 21% of students had declared a disability. Potentially that equates to one in five SLTs in the workforce with a disability, corresponding to the prevalence in the general working age population.
Thinking about how to support colleagues or team members with a disability is something we should all do. SLTs with a disability should be welcomed into the profession and valued for their contribution.
The RCSLT wants to see a workforce that reflects the diversity of the populations it serves. SLTs with a disability can bring valuable experience and understanding to their practice, their service user communities and the workplace.
They may also bring valuable skills such as British Sign Language (BSL) or Makaton, for example, and experience of living with, or being diagnosed with, life-changing conditions.
Those skills are of great value to the SLT profession and it is important SLTs with a disability are supported by employers and within the profession to continue to offer those.
How is disability defined?
In England, Wales and Scotland disability is defined in the Equality Act 2010. This means you’re disabled under the Act if you have a physical or mental impairment that has a ‘substantial’ and ‘long-term’ negative effect on your ability to do normal daily activities.
This can mean anything from a physical or sensory disability to neurodivergencies (including autism) to mental health disorders such as anxiety or depression. There is further detailed guidance on how that is interpreted on GOV.UK.
In Northern Ireland there are two pieces of legislation where disability is defined, they are the Disability Discrimination Act 1995 and the Special Educational Needs and Disability (NI) Order 2005.
A note on terminology
This resource intends to use positive language about disability. Depending on the context, ‘person-first’ terms like ‘an SLT with a disability’ and ‘community-identifying’ or ‘identity-first’ terms like ‘disabled SLTs’ are used.
It is understood that different people have different preferences when it comes to terminology, so this document uses such terms interchangeably. We recommend that when speaking about a person or a group of people, and it is possible to check, you should always use the words that they are most comfortable and identify with.
Ableism (like racism or sexism) is defined as discrimination, prejudice or bias towards a social group; in this case, disabled people. It is based on a belief that typical abilities are superior and more highly valued (Campbell 2009, Wolbring 2008).
This results in treating people unfairly because they have a disability, which might be an illness, injury or a long-term condition. We often unintentionally use ableist language, without realising that this is based on historical prejudices and unconscious biases.
We are listening and learning about this and recognise that we need to continue on this journey. We are committed to welcoming disabled people into our profession and valuing them highly.
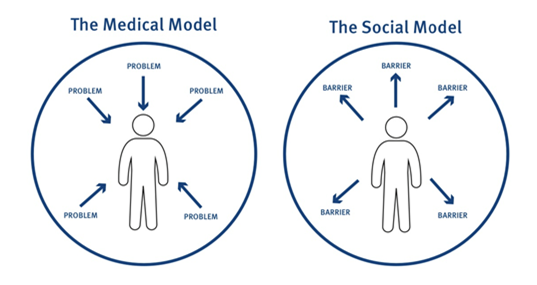
Medical and social models of disability
Historically, disability was seen as a ‘fault’ of the individual and attempts were made to ‘normalise’ people as much as possible using medical interventions. This is known as the medical or traditional model of disability.
From the 1970s onwards, disabled people campaigned for equal rights, citing that environments and attitudes caused disablement, rather than the impairments they had. This is known as the social model of disability.
The theory of the social model is that removing barriers promotes inclusion. The medical model has persisted in the healthcare sector. Studies have shown that this way of thinking about disability is at the root of many issues facing healthcare professionals with impairments as they train and work.
Applying for a job and interview
Deciding whether to disclose a disability and ask for reasonable adjustments at the application or interview stage is a personal decision. There is no need to do so if you do not wish to.
Employers cannot ask job applicants about their health or disability until they have been offered a job, except in specific circumstances where the information is necessary for the application process or a requirement of the job. The Equality and Human Rights Commission provides more information about this.
Employers cannot discriminate at interview or in your application because of disability. But, for example, if you do not request a reasonable adjustment before an interview, then it could be unlikely it could be accommodated at the point you arrive.
The HCPC also provides guidance about looking for work.
There are often local support organisations that may be able to provide support as you decide whether and at what stage to disclose a disability, such as Citizen’s Advice.
Disclosing a disability at an early stage does allow you to take control of that decision and for a more planned approach, rather than feeling more rushed into it at a later point.
Supporting you in your job
It is up to you whether you choose to disclose your disability and who you disclose it to. You will want to think about what you feel comfortable sharing and whether you wish to limit those to whom you talk to about your disability. You may also wish to consider and discuss with your manager whether to disclose your disability to service users or not.
Here are some tips and information from SLTs with a disability about what has been helpful when discussing with their manager and colleagues.
Disability passports
A disability or health passport is a document of needs and agreed adjustments that will follow you around your workplace, including if you change roles. They are helpful in setting out any specific adjustments and in providing a useful structure to follow. As with all plans it is important to review them regularly.
You might find this downloadable health passport from NHS Employers a helpful template to use. Your own organisation may also have one.
Staying well plans
You might also find a staying well plan helpful for you and your manager to complete. It might cover general triggers, things that will be noticeable if you start to be unwell, when to be seriously worried, who to call and who not to call. It can cover how regularly you and your manager should check on your health. It is a live document and should be kept up to date. These documents are useful if the impact of your disability fluctuates.
MIND has produced a useful guide about supporting mental health at work (PDF) which includes advice about what to put in a staying well plan.
Reaching agreement on what is reasonable
Employers must make reasonable adjustments to make sure workers with disabilities, or physical or mental health conditions, are not substantially disadvantaged when doing their jobs.
This applies to all workers, including trainees, apprentices, contract workers and business partners. A reasonable adjustment can take many forms. It might mean adjustments to the working day, the workstation, hours, resources needed, caseload or whether and how the employee can travel.
You and your manager, and possibly occupational health, will wish to discuss any reasonable adjustments that can be made. You may need to discuss more than once to review how these suggestions will work, especially if you are in a new or changed role. Regular reviews should be built in to check whether the adjustments are working as planned.
We have listed some reasonable adjustments that other SLTs with a disability have told us were helpful for them. If you have any other suggestions to add to this list, please let us know.
There are also some useful links in the resources section of this guidance.
Adjustments to facilities and equipment
- Technology to help support you in your work
- Widening a doorway, providing a ramp or moving furniture for a wheelchair user
- Relocating light switches, door handles, or shelves for someone who has difficulty in reaching
Adjustments to enable you to be at work or working
- Phased return after a period of ill health – working fewer days and/or shorter hours
- Working from home until mid-morning if medication leaves you too sleepy to drive
- Working at one place
- Travel accessible by public transport
- Local travel to placements
- Shorter days
- Part-time
- Home working an option
- Having an office day/week (in a role which is mobile) if starting to have early warning signs that health is deteriorating
- Allowing absence from work or training due to treatment, appointments or rehabilitation
Adjustments relating to your role
- Working with a colleague to build confidence, for example on returning from a period of ill-health
- Starting to pick up caseload in stages, eg one school at a time
- Smaller caseloads
- Proof reader of reports
- 1:1 supervision
- Adjustments to training appropriate to the disability
When your disability changes or you have a new diagnosis
If there are changes in your disability or you have been diagnosed with a new disability you will wish to review with your line manager and occupational health.
For a new disability you will need to consider whether your role can still be carried out, with reasonable adjustments if necessary, or whether there are other options such as redeployment that might work.
It is reasonable to expect that you will need time to understand what reasonable adjustments might be required and that both you and your manager will need to work through those as your joint understanding develops. This may take time, and your employer should understand that a period of adjustment to any new condition or change is likely to be required.
If you are a qualified SLT, the HCPC has useful information about when you need to tell them about changes in your health and when it is not necessary.
Raising concerns about disability discrimination
If disability discrimination in your workplace or place of education and training is occurring, whether directed toward you or your service users, the RCSLT is here to help you. All employers and universities have a responsibility to listen and respond.
Take these steps to raise your concerns:
- Refer to your local HR, occupational health or university policies and procedures. They will outline what you should do in the first instance.
- If your concern is about patient care, refer to local service policies.
- Refer to relevant HCPC standards and RCSLT information (eg this guidance and our practice placement guidance).
- Raise your concern with the appropriate person – eg a dedicated officer dealing with disability discrimination, or your line manager.
- If you think your concerns or discussions about reasonable adjustments are not being taken seriously, involve your local Equality Diversity and Inclusion lead or the union.
- If you are a student and your concern is about a placement, raise your concerns immediately so that you can be supported. Do not wait until after the placement has ended, even if you don’t want any action to be taken during your placement. If your concern is about a member of HEI staff, raise your concerns immediately.
- If you are a student, you can raise concerns (relating to placement or your HEI) through your placement provider, academic adviser, personal tutor, programme lead, student support administrator or student services. If you need support when attending meetings, HEIs should have equality, diversity and inclusion (EDI) staff available. If you are unsure of what to do, you can go to the student union for advice.
- The RCSLT has always had a dedicated enquiries line. Members (and students who are not members) can call us to raise concerns or seek advice if the approaches above haven’t worked. Email info@rcslt.org or phone 020 7378 3012 for help.
Tips for managers
If an SLT has a disability then they are permitted in law to ask for reasonable adjustments.
As a manager you may feel concerned about ensuring you do what is legally required or the impact of changes on the team or service users. From the perspective of the SLT, it will have taken courage to speak up about or disclose a disability. It may be the first time they have done so.
A reasonable adjustment needs to work to ensure the member of staff can work and feel valued. So it’s important for both the SLT and manager to take the time to listen and understand each other’s needs at that initial point and proactively work together towards a solution.
It is helpful to consider what is needed from the perspective that it is the absence of adjustments that is the limiting factor in the ability of the SLT to do the job, not the disability itself.
There are significant advantages to diversity in the workforce – people with a disability will bring beneficial skills to a service, for example sign language or Makaton.
A person with lived experience of a disability will have learned resilience and coping mechanisms, have persistence and understand wellbeing management. They will understand and empathise with service users who may experience similar challenges.
This section provides suggestions about responding to requests for reasonable adjustments. Some examples are also provided in the ‘Tips for SLTs’ section. They do not always have to be complex or costly!
Responding to requests for reasonable adjustments
- Don’t make assumptions based on your thoughts about certain conditions or experiences with others who may have that condition. Have a conversation with the employee about how their disability impacts them, as everyone is different.
- Ask what adjustments they think they need, but note that an SLT or student might not know what adjustments they need, especially if the condition is new to them or if the workplace is new to them.
- Include the employee all in emails and conversations where you are trying to sort out reasonable adjustments.
- Be proactive in suggesting you work together on a staying well plan and disability passport if these are helpful.
- Engage occupational health at your local level.
- HR, occupational health, or the staff disability network may have useful suggestions about reasonable adjustments made for others that have been successful.
- Be clear with other team members that reasonable adjustments are not special treatment or an unfair advantage, they are there to provide equity of outcome rather than equal treatment. They are provided to make sure SLTs with a disability are not substantially disadvantaged when doing their job.
- The Government Access to Work scheme can provide practical help for items such as special equipment or other support. The Disability Confident Campaign provides guidance and support for employers of disabled people.
Bradford factor scores
The Bradford factor is a formula used by some HR departments to calculate the impact of employees’ absences on the organisation. It is based on the theory that short, frequent, unplanned absences are more disruptive to organisations than longer absences.
Some employers choose to set thresholds at which Bradford factor scores are deemed to be problematic and require interventions. Employees with disabilities can be adversely affected by such processes and it is therefore important that managers make sure there are safeguards in place to protect employees with medical conditions – such as cancer or mental health conditions – that may cause irregular absence patterns because of hospital appointments.
Employers must make sure that their absence policies do not discriminate against employees with disabilities. For example, it is possible to split Bradford scores and have one for disability related time off and another for other illnesses.
Disclosing a disability and accessing reasonable adjustments flowchart
The flowchart summarises for both SLTs and their managers the steps that can be taken when an SLT discloses a disability. It is important to note that some people may disclose in one setting, but not another – for example, a student may disclose to their university, but not want to disclose for placement – and this is a personal choice.
If you need to have a conversation with your manager to disclose a disability or discuss adjustments and support, ensure that it occurs separately from conversations about your caseload or feedback on your work. You may also bring an advocate, such as a family member, friend, union member, or paid advocate.
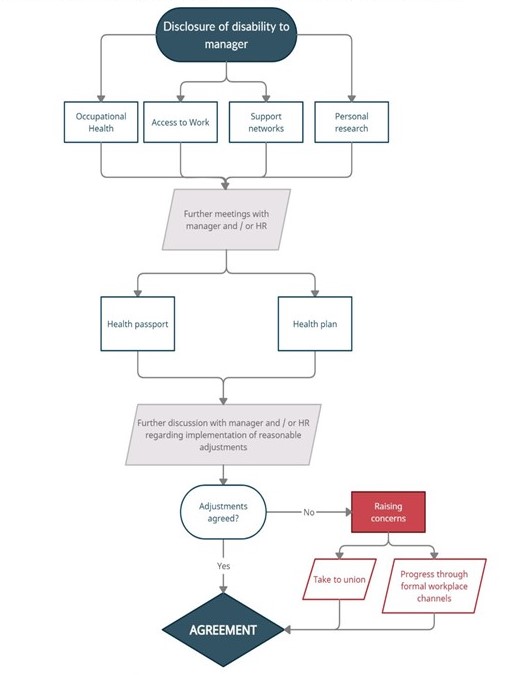
Flowchart outline
- Disclosure of disability to manager
- Occupational health
- Access to work
- Support networks
- Personal research
- Further meetings with manager and/or HR
- Health passport
- Health plan
- Further discussion with manager and/or HR regarding implementation of reasonable adjustments
- Adjustments agreed?
- If yes, form agreement
- If no: raise concerns
- Take to union
- Progress through formal workplace channels
- Form agreement
The RCSLT has a dedicated enquiries line. Members can email info@rcslt.org or phone 020 7378 3012 to seek advice if the approaches outlined here haven’t worked.
Students on placement
It is worth noting that around 21% of SLT students have declared a disability. The RCSLT wants to see increased diversity in the profession so that it is more reflective of the populations it serves.
We want to encourage students with a disability into the profession and support them through their training. They can bring valuable lived experience and understanding to their learning, practice and the workplace. They may also bring in-demand skills such as BSL or Makaton, and experience of living with or being diagnosed with life-changing conditions.
They are likely to have learned how to manage their disability while juggling their education, and been successful in reaching the high standards required for entry into HEIs. That resilience is of great value to the SLT profession and it is important that students with a disability are supported by employers as they enter workplaces, often for the first time.
If you are a placement educator, you will be aware that students with a disability coming into the workplace on placement may also declare their disability and require reasonable adjustments to be made.
Comprehensive guidance on this can be found in the RCSLT’s practice based learning guidance. The information on this page provides additional information to support how you and placement students can use and implement the guidance in a practical manner.
We are aware that some students with a disability have had comments made to them while on placement, such as “you won’t be able to cope once you qualify”, “you are a client, not an SLT” or similar comments. It is important to emphasise that these are not acceptable or appropriate comments to make to a student, and it is not the place of the practice educator or other colleagues to make a judgement of this nature.
If you are a student with any disability, please read this section and think about how it might apply to you and help you with decisions about your placement.
Disclosing a disability prior to placement
Students with a disability may already be aware that workplaces are required to make reasonable adjustments if requested. See previous sections of this guidance for information about reasonable adjustments.
However, we know that it can be daunting to work through the practicalities of making a request. You might want to think about the following:
- As a student it is your decision about whether you disclose a disability, whether to your university or to your placement provider, and it may be difficult to weigh different aspects of that decision. You are not required to disclose a disability to your placement provider, even if you have already disclosed it to your university. This said, the HCPC also provides a student code of conduct, which states: “provide, as soon as possible, any important information about your conduct, competence or health to your education provider and practice placement provider”. There is clearly a tension between these two points to work through that will be different for each individual and their circumstances.
- Even if you think you won’t need adjustments or don’t want to ‘cause a fuss’ we would strongly encourage you to discuss with your university if you feel able. Often there will be a clinical coordinator who can help – you can find out via your personal tutor if unsure. All universities have their own processes, so ensure you find out how they work in yours.
- Any workplace placement educator will know about the requirement to provide reasonable adjustments if you ask for them. They are likely to already have experience with students with a disability, or may have a disability themselves.
- Even if you disclose a disability to your university, they need your permission to share that information with a placement workplace.
Allow enough time
If you think you may wish to disclose a disability before a placement, allow plenty of time for discussion of reasonable adjustments and exploration of the potential needs. Formal processes can be slow, so think months, rather than days or weeks, ahead. It is not too early to discuss reasonable adjustments immediately when you start your course.
Who to talk to
You may have already spoken to your personal tutor about your disability. But it is worth also speaking directly to the clinical coordinator or person arranging placements at your university. It can be a complex process, so it is best practice for students to be supported by their university if they then decide to disclose a disability to their placement workplace.
Why it may be beneficial to disclose a disability
The decision on disclosure will be a personal one and no two situations will be the same. For some people it may be better not to disclose a disability – perhaps, having had a discussion with the university, the placement can be flexible with times or locations and that will be sufficient without disclosing to the placement provider. The university cannot tell the workplace about a disability unless they have your permission to do so.
In other situations it may be strongly advisable to disclose a disability to the placement provider so reasonable adjustments can be put in place to ensure equity of outcome for students with a disability. Placement providers are unlikely to be able to introduce adjustments with little notice or once the placement has started (unless the disability is new, for example).
Take a look at our case studies of students’ experiences.
Accessing reasonable adjustments and support on placement
Support from university disability services and application of existing plans or passports
You may be able to take any existing reasonable adjustments agreed with your university and use them as a basis for discussion with your placement provider. However it is important to consider how the workplace will differ from the university environment and it is possible that amendments will be needed.
Discussions about reasonable adjustments
It is best practice to separate discussions on reasonable adjustments from those of professional practice, performance or caseload. There should also be care to ensure that communications between the university and placement provider are anonymised as appropriate to ensure confidentiality.
Flexibility and customisation
The purpose of adjustments is to provide equity of outcome for a student with a disability. It is not about giving those students any sort of advantage. Adjustments need to be customised to the needs identified and flexible if the disability has variations in its impact on the student.
It should not be assumed that the student will know exactly what adjustments are needed, if for example the environment is new to them or the disability is new to them.
Resolving issues that arise on placement
If a problem arises on placement the RCSLT practice based learning guidance makes clear that any party (student, HEI, practice educator) can request a triumvirate meeting to adapt the reasonable adjustments.
Where to find support
- University occupational health
- Other university teams, eg neurodiversity, mental health
- Networks – as a student or a placement educator, local support groups may exist that would provide information and informal support; for example, NHS diversity networks, university groups, RCSLT networks.
- As a placement educator, you might also find it helpful to contact the EDI lead in your Trust or organisation (if you are in an NHS or other public setting).
Colleagues and allyship
We hope that all SLTs can be allies to SLTs with a disability. As SLTs you can build relationships of trust with marginalised individuals and/or groups of people.
Although you might not be a member of an under-invested or oppressed group, you can support them and make the effort to understand their struggle and use your voice alongside theirs.
The NHS provides a programme and resources relating to allyship.
Useful links and resources
Case studies
Government and human rights
- Equality and Human Rights Commission
- GOV.UK: Access to work
- GOV.UK: Work and disabled people
- Equality and Human Rights Commission: Employing people: workplace adjustments
The Health and Care Professions Council (HCPC)
Your rights and employer obligations
- Acas (the Advisory, Conciliation and Arbitration Service): Supporting mental health at work
- Health and Safety Executive (HSE): Mental health conditions, work and the workplace
- NHS Employers: Reasonable adjustments in the workplace
Charities, third sector and other links
- Difference: charity representing disabled people in the North East of England
- Life of Pippa: a blog and book about being a university with a chronic illness
Mental Health in the Workplace
General guides to mental health at work
- Mental Health Foundation: How to support mental health at work
- Mental Health UK: five top tips for mental wellbeing guide
- Total Wellness: how to stay mentally healthy at work
- Employee Benefits: Tips to stay mentally healthy at work
COVID-19 specific advice
- City Mental Health Alliance: Supporting colleagues to stay mentally healthy in unusual working conditions
Tips for employees
- Mind: How to be mentally healthy at work
- Mind: Top tips for staying well at work
- SAMH (Scotland’s national mental health charity): be mentally healthy at work guide
Discrimination at work due to mental health
- Mind: examples of discrimination at work
- High Speed Training: What To Do If You Suspect Mental Health Discrimination at Work
Tips for employers
- Mind: how to support staff who are experiencing a mental health problem (PDF)
- Heads Up: Managing someone with a mental health condition (PDF)
Trade unions
- TUC: Autism in the workplace
- Unite: Disabled members in Unite
Documentaries
- Silenced: The hidden story of Disabled Britain (BBC iPlayer)
For more than a century, one group of people in Britain has been shut out of society, denied basic human rights and treated with fear and prejudice. In this shocking, moving film, Cerrie Burnell is going to uncover the hidden story of how disabled people fought back – and won their freedom. Now, she wants to find out where these attitudes to disabled people come from and why they persist today. - Targeted: The Truth about Disability Hate Crime (BBC iPlayer)
A film about the routine aggression and abuse faced by disabled people in today’s Britain, from verbal name-calling to violent physical attacks. Featuring a wide range of testimony from survivors.
Related content
Case studies
Experiences of student SLTs with a disability
Practice-based learning guidance
Reasonable adjustments on placements
Diversity, inclusion and anti-racism
Support and resources for SLTs
